Ethnomedicines and Health Management in Kenya: Which Way Forward?-Juniper Publishers
Juniper Publishers
Ethnic diversity and ethnosystematics have gradually evolved to give rise to unique cultures and ethnomedical practices and systems that have withstood the test of time worldwide. An estimated 70% of Kenyans rely on ethnomedicines as the only source of healthcare, with up to 90% using medicinal plants and animals as part of any treatment process. WHO estimates that as many as 70-95 % of the world’s people especially in developing countries rely on ethnomedicines for their primary healthcare needs and henceforth its recommendation in the Alma-Ata Declaration adopted by WHO and UNICEF in 1978 for its integration into primary healthcare systems, particularly of developing countries if the objective of the “Health for All by the Year 2000” was to be realized [1]. While about 100 million people use ethnomedicines in the European Union (EU) alone while more than one third of Americans and Europeans use assorted herbs for healthcare purposes, spending over £7.0 billion annually. On other hand, 1.5 billion people use Chinese Tradition Medicine worldwide and most modern conventional drugs have their origin of use and application deeply rooted in ethnomedicines. There is need therefore to understand the holistic nature of ethnomedicines so that it can be easily utilized and applied. This overview focuses on the composition and understanding of ethnomedicines, its historical development in Kenya, its challenges and finally suggests a way forward of unlocking its potential together with anticipated benefits. An illustrated example of unlocking potential of ethnomedicines is briefly given for Maasai Mara University with reference to its African Medicinal Botanical Garden under development.
Keywords: Ethnophamacology; Conventional medicine; Legal framework of ethnomedicines; Healthcare systems; Ethnopractitioners
Introduction
Ethnic diversity and ethnosystematics have gradually evolved to give rise to unique and beneficial cultural and ethnomedical practices that have withstood the test of time in various human societies worldwide. The prospect of the sustainable growth, development and evolution of these ethnopractices (including social, cultural and religious practices) has been achieved due to a rich biological diversity closely associated with diversified ethnicity in which each existing ethnic grouping contributes a unique and yet useful ethnopharmacopoeia [2]. Achieving optimal wellness for humanity together with animals, minerals, soils, water, microorganisms, plants and the entire environment that humans take care, has ever remained the omnipotent challenge since antiquity! The aim of these ethnopractices therefore was to develop a pool of ethnomedicines that approximates to the aspirations and realities of a holistic approach to ill-health condition of humanity and the entirety wellbeing rather than the conventional curative mechanism of technological fix of specific diseases only [3,4]. Moreover, the packaged ethnotreatments take care of the environments in which the target organisms exist, thus making ethnomedicines very unique and indeed fulfilling as ethnopractitioners endeavour to reconnect the individual-based social wellbeing and emotional equilibrium of a target patient whose taboos, norms and other traditions are philosophically considered alongside the ethnic code of conduct, governing set of rules and existing relationships [5]. As Abdullahi [2] stated, in many circumstances, the ethnopractitioners normally and more often than not act as, “an intermediary between the visible and invisible worlds; between the living and the dead or ancestors, sometimes to determine which spirits are at work and how to bring the sick person back into harmony with the ancestors and/or spirits”. Ethnomedicines have proved powerful ingredients in our livelihoods at all levels as a reliable, independent and biologically evolving healthcare system since human existence [6]. For incidence, an estimated 70% of Kenyan’s rely on ethnomedicines as the primary source of care, with up to 90% using animals, minerals, soils, water, microorganisms and plants as part of any treatment process. While World Health Organization (WHO) estimates that as many as 70-95% of the world’s people especially in developing countries rely on ethnomedicines for their primary healthcare needs and henceforth its recommendation for integration into primary healthcare services [5,6]. And further estimates that about 100 million people use ethnomedicines in the European Union (EU) alone while more than one third of Americans and Europeans use assorted herbs for healthcare purposes, spending over £7.0 billion annually. While China estimates that about 1.5 billion people globally use the Chinese Herbal Medicines (CHM) [8,9]. There is also an estimate of over 50% of modern pharmaceutical drugs having their origin of use and technological applications in ethnomedicines, with plant species together with the ethnopractitioners that use them taking the lead as the main resources [10-19]. Nevertheless, the most disturbing picture is that out of an estimated number of about 390, 800 plant species known in the world today, only 15% of these plant species have been investigated for possible medicinal value. How about the medicinal value of more than 1.611 million existing zoological species so far named and described and another estimated number of about 10 to 30 million living organisms that remain to be discovered? This is just amazing and an incredible pharmaceutical resource that is yet to be utilized to benefit humanity worldwide! This aforementioned brief account on ethnomedicines and health management therefore provides an adequate amount of evidence for investment into ethnomedicines research and development with a view to identifying more resources for developing new pharmaceutical agents and adding value to the existing ethnomedical agents and practices in Kenya [20]. This overview of ethnomedicines outlines its composition and understanding, its historical development in Kenya, its challenges and finally suggests a way forward of unlocking its great potential together with anticipated benefits.
Composition of Ethnomedicines and Names Uniquely Used for Describing and Defining it
Ethnomedicines is uniquely defined and variously described using a wide range of geographic- and ethnic-based terminologies worldwide such as, Ayurveda, Siddha medicine, Unani, ancient Iranian medicine, Iranian (Persian) traditional medicine, Arabic indigenous medicine, Islamic medicine, traditional Chinese medicine, traditional Korean medicine, ancient Greek medicine, Haitian folk medicine, Native American traditional herbal medicine, Uyghur traditional medicine, Irish medical families, Japanese Kampō medicine, traditional Aboriginal bush medicine, Georgian folk medicine, acupuncture, Celtic traditional medicine, Muti, Ifá, native healing powers and traditional African medicine (ancient Egyptian medicine). Other descriptive terminologies of ethnomedicines include: traditional medicine, folk medicine, indigenous medicine, natural medicine, home remedy (granny cure), herbal medicine, integrative medicine, complementary medicine, anthroposophic medicine (massage, exercises, counselling and substances from plants, animals, soils, water, minerals, microorganisms etc.), alternative medicine, pseudo-medicines, magical medical practices, quackery medical practices, homeopathy, skepticism, etc. Ethnomedicine industry is therefore marred with a lot of controversy, doubt, suspicion and skepticism, which do not ensure efficiency, sustainability, effectiveness and timeliness in service delivery in the entire industry, henceforth its failure to grow and develop. This haphazard consideration of the field of ethnomedicines shows that this particular discipline has not grown and developed across board uniformly and that it has not professionally curved its own niche and thus gotten into the mainstream administration of academia and research. However, given that WHO is a specialized agency of the United Nations leading and setting out the course for the use and application of ethnomedicines throughout the world, it has universally developed the most acceptable and favourable definition of ethnomedicines as, “the sum total of the knowledge, skills, and practices based on the theories, beliefs and experiences indigenous to different cultures, whether explicable or not, used in the maintenance of health as well as in the prevention, diagnosis, improvement or treatment of physical and mental illness” [7]. Throughout the entire text of this manuscript, the meanings of the following terminologies have been understood to be in the following context unless otherwise differently explained.
A Critical Review of Concepts and Definitions of Fundamental Terminologies
Ethno
A prefix used in the formation of compound words in English language to mean the study of races, people, cultures, tribes, caste systems, nations, societal classes and societies with a common and distinctive origin and evolution in terms of language, communication, cultural practices, nutrition, norms, beliefs, taboos, traditions, skills, technologies, innovations and just the entire livelihood from its ancient times to current. Examples include: Ethnomusicologistsomeone who studies the music of different societies and cultures, Ethnocentric-believing that the people, customs, and traditions of your own race or nationality are better than those of other races and Ethnology-the study of different societies and cultures
Ethnography
A scientific description of cultures (including traditional knowledge, ethnopractices and customs of indigenous/native and local people) of a particular society by someone who has lived in it and/or a book containing such information.
Ethnobotany
The scientific study of the traditional knowledge, practices and customs of indigenous/native and local people of a given geographical location and/or ethnic grouping concerning the values, applications and wider practical utilization and interaction of plant species by humanity; including their clothing, construction, ornamental, initiation ceremonies, farming, nutritional, medical, religious and many other aspects of uses in the course of their life [2,21,22].
Herbalism
A traditional medicinal or folk medicine practice based on the use of plants and/or plant extracts intended for medicinal purposes or for supplementing a diet (nutraceutical) with the aim of providing healing effects. Herbalism is also variously known as botanical medicine, medical herbalism, herbal medicine, herbology and phytotherapy.
Phytotherapy
From the Greek, “phyton” meaning “plant” and “therapeuein” meaning “to take care of, to heal,” this is the term used to describe medical herbalism too, is a science-based medical practice of using plant-derived medications in the treatment, management and prevention of diseases based on their empirical evidences of their medical potential and value [23].
Zoopharmacognosy
Is a broad terminology referring to a natural-based behaviour in which non-human animals apparently self-medicate by selecting and ingesting, absorbing or topically applying plants, soils, insects and psychoactive drugs or humans using animals, animal parts and products to prevent and/or therapeutically to reduce the harmful effects of pathogens and toxins as prophylactic and/ or curative measures, respectively [24-27]. This terminology originated from the Greek roots, zoo (meaning, “animal”), pharma (meaning “drug”) and gnosy (meaning “knowing”) and ever since its origin in 1993, it has found its position in the mainstream of administration of academia and research as independent discipline [27-29]. It involves what Caroline Ingraham described in 1984 as “evolution of animals’ behaviour to cope with potential health threats including disease and injury, through the development of solutions to restore health by self-diagnosing and administering medicinal compounds naturally found in the immediate environment.” Nevertheless, Ingraham’s philosophical statement of Applied Zoopharmacognosy has been heavily criticized by the author of The Skept Vet (http://skeptvet.com/Blog/2016/10/the-natural-nonsense- that-is-applied-zoopharmacognosy/).
Geophagy (with ethnomedicinal and nutraceutical values) (also known as geophagia)
The practice, in some world tribal and ethnic societies of eating earthy substances (such as clay) that in humans is performed especially to augment a scanty or mineral-deficient diet or as part of a cultural tradition that is associated with ethnomedicinal value and/or bodily requirements of organisms [30-32]. From different viewpoints, geophagy has been regarded as a psychiatric disease, a culturally sanctioned practice or a sequel to poverty and famine [31,33].
Microorganisms as ethnomedicines
The search for drugs from microorganisms to manage human health and that of other organisms is more recent and not based on ethnomedicinal root records in time and space as is associated with evolutionary history of humans [34]. Probably of particular significance to note is a considerable part of the currently available conventional pharmaceuticals in clinical use being comprised of drugs derived from microorganisms too [13]. Through the practice of geophagy therefore, humans may be consuming a lot of microorganisms unknowingly and henceforth, benefiting greatly from their useful natural compounds available in the soils with curative, protective and preventive properties [32]. It follows with logical necessity that a considerable part of the medicinal value of soils may be attributed to the existence of these microorganisms as soil-based bioresources with medically useful compounds.
Ritual medicines
In this context, it refers to a sequence of activities and/or events practically involving gestures, words (utterances, known as performatives) and objects performed in a sequestered place and according to set sequence of social custom, taboos and/or normal protocol, more often as part of a traditional religious ceremony in performing divine and/or holy services but with a view to getting holistic curative, protective and preventive remedies [35-37]. Ritual is more related to performing religious services as a methodological measure of religiosity level although characterized by formalism, traditionalism, invariance, rule-governance, sacral symbolism and performance [36,38,39]. It is full of genres and anthropological theories that govern human evolutionary processes in the society [40-42].
Complementary medicine (CM)
The terms “complementary medicine” or “alternative medicine” refer to a broad set of health care practices that are not part of that country’s own tradition or conventional medicine and are not fully integrated into the dominant healthcare system. They are interchangeably used with traditional medicine in some countries.
Spirituality
It explores life purpose/meaning and relates to religious conviction, involving deep feelings or beliefs of a religious nature and the quality of being concerned with the human spirit or soul (and/ or mental or emotional communion) rather than the material or physical values or pursuits in life. However, religion and spirituality are not the same thing, nor are they entirely distinct from one another but the two are closely related and may offer questions and answers about the infinite, provide support during emotional crises and invoke a sense of awe, wonder, and reverence. Conversely, life issues relating to comfort, beliefs, reflection, ethics and awe are all common to both religion and spirituality, thus affecting the way one think, feel and behave in the society. Nevertheless, Mastin [43] defined spirituality as, the measure of how willing we are to allow Grace (loveliness)-some power greater than ourselves-to enter our lives and guide us along our way, thus being how loving you are, how unconditionally accepting you are toward yourself and others. Spirituality takes charge of one’s emotional health and wellbeing (a state of being in alignment (body, mind, and spirit)) and refers to the way individuals experience their connectedness, energization, contentment and balancing to the moment, to self, to others, to nature and to the most significant or sacred and/or supernatural powers.
Divinity
In religion sense, divinity or godhead is the state of things that are believed to come from a supernatural power or deity (holy being), such as a god, goddess, Supreme Being, creator deity or spirits and are therefore regarded as sacred and holy. Such things are regarded as divine due to their transcendental origins or because their attributes or qualities are superior or supreme relative to things of the Earth. Divine things are regarded as eternal and based in truth, while material things are regarded as ephemeral and based in illusion. Such things that may qualify as divine are apparitions, visions, prophecies, miracles, and in some views also the soul, or more general things like resurrection, immortality, grace, and salvation. Otherwise what is or is not divine may be accordingly defined based on the ethnicity, beliefs, lifestyle, religiosity levels and at times, personality and environmental situation in one’s life. Above all, supernatural powers and associated holiness and being sacred in divinity make sense in an ordinary life when it provides holistic curative, protective and preventive remedies in ill-health situations in the society [35-37].
Ethnoknowledge systems (such as Ethnobotany, Ethnozoology, Witchcraft, Ethnomedicines, Ethnography etc)
Is geographic and/or ethnic-based traditionally defined complex body of knowledge (information), practices, norms, taboos, cultures and believes that normally guide day-to-day livelihoods of individuals belonging to a specific geographic location and/or ethnic grouping regarding their socio-cultural wellbeing, health, leadership, governance, economic life, relationships, informal education etc. The coherent ensemble of this complex body of knowledge (information), practices, norms, taboos, cultures and believes is build up from a wide range of sources (inherently within and without) in time and space throughout the evolutionary history of that particular geographic location and/or ethnic grouping [44,45]. The holistic nature and interconnectedness of ethnoknowledge systems in human societies in which they exist, make them very unique, to be held in high esteem, independent and as a fundamental resource for growth and development of ever evolving humanity. It therefore follows with logical necessity that the efficiency and efficacy of every defined athenahealth system may be appropriately and favorably measured in a culturally appropriated way, and the failure to consider the existing cultural context and framework within which it operates may result in its misunderstandings and failure to achieve the desired results [46- 48].
Cultural life
Refers to upholding the professional ethics of ethnopractices, ethnomedicines, ethnoknowledge, norms, taboos, cultures and believes of the various components of ethnoknowledge systems within any one given existing cultural context and framework. Culture itself is the sum total of people’s way of life through evolutionary history since antiquity, thus referring to their entire social behaviour, mindset ethnic-based orientations and norms (informal understandings that govern the behaviour of members of a particular society) found in human societies and expressed in all sorts of forms, both physically (objects and architecture they make or have made) and immaterially (values, belief systems, attitudes, rules, norms, morals, language, organizations, and institutions) [2]. Culture also considers values of the people and the ways they think about and understand the world around them and their own lives [49,50].
Ethnosurgery mechanisms and fracture making
Is a highly evolved and specialized form of traditional medicine that breaks bones to remove bad areas and restores bone tissues to their original physical and mechanical properties using plants and their extracts and poultice together with splint without cast and with the application of systematic massage [51-56]. The use of natural products, majorly plant-based in healing bone fractures is an indicator that phytochemicals may be developed as potential therapy for facilitating the healing process of bone fractures [57]. Nevertheless, how traditional medicine achieves a highly sophisticated kind of postnatal regenerative process that recapitulates many of the ontological events of embryonic skeletal development [58], has ever remained a mystery to many observers!
Ethnopsychotherapy
Also called Traditional Psychotherapy, just like any other types of therapies, aims to mitigate social, developmental, behavioural and emotional difficulties and irrational thoughts, beliefs, cognitions, behaviours and feelings by use and application of the knowledge of the science of behaviour and mind, including conscious and unconscious phenomena, as well as feeling and thought to interact with another affected person to help change the person and overcome problems in desired ways [59,60]. The rationale of undergoing psychotherapeutic processes is to continuously improve an individual’s well-being and mental health, to resolve or mitigate troublesome behaviours, beliefs, compulsions, thoughts, or emotions and to improve relationships and social skills of the affected person in the society while integrating mind, heart, body and spirit but not spirituality unless it is regarding bereavement [61-64]. Certain psychotherapies are considered evidence-based for treating some diagnosed mental disorders in life of certain individuals [64-68].
Phytonutrients
(also called phytochemicals, originates from the Greek word, “phyton” meaning “plant” and from the Latin word, “nūtrīre” meaning “nourish”. These are substances found in certain plants, which are believed to protect plants from damaging environment in which the plants exist and are beneficial to human health and help prevent various diseases. Plant foods contain thousands of natural chemicals, which help protect plants from germs, fungi, bugs, and other threats. Phytonutrients aren’t essential for keeping one alive, unlike the vitamins and minerals that plant foods contain. But when you eat or drink phytonutrients, they may help prevent various diseases and keep your body working properly. Examples include carotenoids, ellagic acid, sulphides, thiols, flavonoids, Proanthocyanidins, flavan-3-ols, resveratrol, phytosterols glucosinolates, anthocyanins, lycopene, phytoestrogens etc., obtained from foods such as fruits, vegetables, herbs and spices including whole grains, nuts, beans, tomatoes, tea, tofu, dates, peppermint, cloves, berries, olives, nutrition-rich onions, leeks, grape juice extracts, cranberries, cocoa, strawberries, nutrition-loaded tomatoes, carrots, sweet potatoes, coffee, garlic, beets, black pepper, cardamom, blueberries, broccoli, asparagus, dandelion tea, earl grey tea, wine, chai tea and green tea are examples of foods high in phytonutrients. Phytonutrients are the basis for more than 40 percent of medications today and have become a great resource of treatment of a wide range of diseases such as pulmonary and cardiovascular diseases, diabetes, obesity and cancer. Phytonutrients also provide colour, flavour and smell to plants. Medicinal plants that are high in phytonutrients include: aloe vera, arnica, arrowroot, milk thistle, clove, dandelion, ginkgo biloba, ginseng, lavender, peppermint, St. John’s wort, Witch Hazel etc.
Nutraceuticals
Are products derived from food sources that are purported to provide extra health benefits, in addition to the basic nutritional value found in foods. Nutraceutical products have been found to prevent chronic diseases, improve health, delay the aging process, increase life expectance and support the structure or function of the body.
Traditional Birth Attendants (TBA)
Also known as a traditional midwife, community midwife or lay midwife, is a pregnancy and childbirth care provider who assists a woman during labour and delivery with skills learned by apprenticeship or personal experience rather than by formal training [69]. Traditional birth attendants provide the majority of primary maternity healthcare in many developing countries and may function within specific communities in developed countries [70,71]. Traditional midwives provide basic healthcare, support and advice during and after pregnancy and childbirth, based primarily on experience and knowledge acquired informally through the traditions and practices of the communities where they originated [72-74]. Many traditional midwives are also herbalists, or other traditional healers in their own unique ways. They may or may not be integrated in the formal healthcare system and sometimes serve as a bridge between the community and the formal health system and may accompany women to health facilities for delivery [69,75].
Anthroposophic medicine (massage, exercises, counselling and substances from plants, animals, soils, water, minerals, microorganisms etc.)
Anthroposophic medicine (or anthroposophical medicine) is a form of alternative medicine. Devised in the 1920s by Rudolf Steiner (1861-1925) in conjunction with Ita Wegman (1876- 1943), anthroposophical medicine is based on occult notions and draws on Steiner’s spiritual philosophy, which he called anthroposophy. Practitioners employ a variety of treatment techniques based upon anthroposophic precepts, including massage, exercise, counselling, and substances [76-78].
Naturopathy or naturopathic medicine
Is a form of alternative medicine that employs an array of pseudoscientific practices branded as “natural”, “non-invasive”, and as promoting “self-healing”. The ideology and methods of naturopathy are based on vitalism and folk medicine, rather than evidence-based conventional medicine. A Naturopath is a health practitioner who applies natural therapies. Her/his spectrum comprises far more than fasting, nutrition, water, and exercise; it includes approved natural healing practices such as Homeopathy, Acupuncture, and Herbal Medicine, as well as the use of modern methods like Bio-Resonance
Homeopathy
Is a system of alternative medicine created in 1796 by Samuel Hahnemann, based on his doctrine of like cures like (similia similibus curentur), a claim that a substance that causes the symptoms of a disease in healthy people would cure similar symptoms in sick people? Homeopathy, or Homeopathic Medicine, is the practice of medicine that embraces a holistic, natural approach to the treatment of the sick. Homeopathy is holistic because it treats the person as a whole, rather than focusing on a diseased part or a labelled sickness.
Milestones in Ethnomedicines Industry in Kenya:Legislative and Regulatory Framework
It is not exactly known with certainty when humans started practicing ethnomedicines but documentations indicate early records began some 4000 years ago [79] and it may be as old as human history on the Planet Earth. Nevertheless, since pre-historic times, ethnomedicine industry within the various ethnoknowledge systems and ethnic-based cultural settings provided the only sources of healthcare systems worldwide, Kenya included [48,80- 82]. Therefore, since antiquity, this form of healthcare system was well established and unequivocally trusted to take care of any nature of ill-health in human environments [83-86], as its method of discovery must have presented a lot of challenges to these early humans who turned to be guinea pigs in the “laboratory” (in this case, bushes and/or homesteads) for testing. Risks involved consuming poisonous material that resulted into physical damage (both internal and external), chronic diseases, vomiting, diarrhea, coma and even death [20]. By this strategy, the early humans dis covered a variety of food stuffs from plants as well as a wide range of natural medicines [87]. Following scientific evolution and revolution, particularly from 15th Century provided an evidence-based standard of medication and the entire healthcare systems that gave birth to conventional medicine that spread around the world through missionaries, colonialism, slave trade and recruitment to participate into world wars took place [88]. Unfortunately, the spread of conventional medicine occurred at the expense of ethnomedicine industry, which was in return, severely condemned. In reality therefore, this conventional medicine should be the Alternative medicine and vice versa. For instance, in Kenya, the Colonial 1910 Medical Practitioners and Dentists Ordinance therefore did not recognize ethnomedicine industry as a result of its international condemnation and wholesome dismissal and henceforth, total rejection. Rejection of ethnomedicine industry continued post-colonial era with the succeeding African governments, for instance in Kenya, ethnopractitioners were continually condemned in 1969 by former President, the late Mzee Jomo Kenyatta, who did not want to embrace the practice of ethnomedicines at any level, albeit being brought up in such an environment under the care of ethnopractitioners. This was a case of the influence of the western powers on succeeding African governments, a manifestation of the importation of the European law (English Common Law) into Africa that experienced conflict between the foreign law and the indigenous African customary rules, norms, taboos, culture and heritage as the case of Kenya’s Witchcraft Act (Cap. 67) that came into force on 12th November, 1925, Uganda’s Witchcraft Act (Cap. 108) that came into force on 28th March, 1976 and the Tanganyika’s Witchcraft Ordinance (Cap. 18) that came into force on 28th December, 1928 [89]. Noted that these laws were completely rejected as they failed to take into account the customary rules, heritage and socio-economic ethos of the people of East Africa that they were supposed to regulate, notwithstanding the existence of other institutions for their enforcement. It is important to note that these laws were introduced to condemn the practice of ethnomedicines as was equated to witchcraft by the then colonial masters throughout the entire of East Africa region. By this kind of intimidation, the ethnopractitioners were practically threatened and put in a position of dilemma where they could not be able to provide culturally competent and appropriate healthcare services to their clients [90]. Following this reaction, many ethnopractitioners abandoned their work at the expense of Christianity, Islamic and other religious faith and being loyal to the then ruling political regime, a situation that led to the underdevelopment of the entire industry of ethnomedicines.
A. However, the state of affairs of the use and application of ethnomedicines drastically changed when World Health Organization (WHO) realized the value and importance of ethnomedicines in healthcare systems, particularly in Primary Healthcare System of the developing countries [1] Following this realization, ethnomedicines was incorporated into Kenya’s national health policy framework in the late 1970s following the Alma-Ata Declaration, adopted by WHO, UNICEF in 1978 [1], from where it was resolved that traditional medicine had to be incorporated in the healthcare systems of developing countries if the objective of the “Health for All by the Year 2000” was to be realized. “Although traditional medicine has been used for thousands of years and has made great contributions to human health, the Alma-Ata Declaration was the first recognition of the role of traditional medicine and its ethnopractitioners in primary healthcare by WHO and its Member States and Governments”, noted by WHO secretariat. However, African countries did not seriously consider this declaration as important as WHO itself. Nevertheless, Member States and Governments and WHO governing bodies, Kenya included, have adopted a number of resolutions and declarations on traditional medicines ever since the Alma-Atta Declaration of 1978 [1] and have differently impacted on member states and governments include the following noted milestones with special reference to World Health Organization where possible: a) In 1984, a Traditional Medicines and Drugs Research Centre (TMDRC) was established as part of the Kenya Medical Research Institute (KEMRI) to help validate the use and practice of ethnomedicines. For the last 24 years, TMDRC focused on research and development (R&D) without special attention to capacity building component at all levels and embracing the continuum of togetherness for specifically, strategic promotion of the sustainable use and practice of ethnomedicines amongst local and native communities. b) Kenya’s Development Plan 1989-1993 (34) recognized ethnomedicines and made a commitment to promote the welfare of ethnopractitioners who were condemned in 1969 by the then, President, the late Mzee Jomo Kenyatta. c) In 1999, Kenya’s Patent Law was revised to include protection for traditional medicines and its practices. d) Following WHO affirmative action, the Member States and Governments of the WHO African Region adopted a resolution in Ouagadougou, Burkina Faso, in August 31st, 2000 called “Promoting the role of traditional medicine in healthcare systems: A strategy for the African Region Committee.” This strategy provided for the institutionalization of traditional medicine in healthcare systems of the member states and governments of the WHO African Region. e) In Lusaka in July 2001, the Organization of the African Unity (OAU) Heads of State and Government declared the period 2001 - 2010 as the African Decade on African Traditional Medicine. f) In May 2002, World Health Assembly (WHA) launched the first ever WHO Strategy on Traditional Medicine 2002-2005 to help guide states and governments in developing legal framework that can help in integrating traditional medicine into primary healthcare systems. g) In May 2003, WHA made resolutions to promote traditional medicine, including WHA56.31.
h) In July 2003 in Maputo, the African Summit of Heads of State and Government was held and endorsed the plan of action for implementation of the Decade of African Traditional Medicine declared in Lusaka in July 2001 and the institution of the African Traditional Medicine Day in Member States to be celebrated every year on 31st August with effect from 2003. i) In 2005, National policy on Traditional Medicine and Medicinal Plants was drafted and emphasized the need to take inventory of all the medicinal plants in the country. It also sought to encourage the setting up of nurseries and herb gardens with the ultimate goal of bio-conservation and research. Unfortunately, these recommendations are yet to be passed into law by the Kenyan parliament [91]. j) In May 2008, the National Coordinating Agency for Population and Development (NCAPD), a semi-autonomous Kenya government agency that promotes and coordinates population and development activities in Kenya, developed a policy brief No. 1, Seeking Solutions for Traditional Herbal Medicine: Kenya Develops a National Policy. This policy brief summarized the major issues requiring consideration as Kenya worked to develop a national policy for guiding, promoting and regulating traditional medicine in the country. k) On 26th June, 2008 African Ministers of health and heads of delegation of African countries met in Algiers for the Ministerial Conference on Research for Health in the African Region and adopted The Algiers Declaration in which they agreed to promote research in traditional medicine and strengthen health systems while taking into account the socio-cultural and environmental situation in which the people of Africa live. l) In November, 2008, the first WHO Congress on Traditional Medicine, 7-9 November 2008, Beijing, People’s Republic of China was organized by WHO to further assess the role of Traditional Medicine/Complementary/Alternative Medicine (M/C/ AM), to review the progress of countries and to help Member States integrate TM/C/AM into their national healthcare systems. m) On 8th November, 2008, The Beijing Declaration was adopted to promote the safe and effective use of traditional medicine, and to call on WHO Member States and other stakeholders to take steps to integrate TM/C/AM into national health systems. n) In 2009, WHA resolution on Traditional Medicine was adopted on behalf of member states and governments (WHA62.13, 2009). o) In July 2009, The National Policy on Traditional Knowledge, Genetic Resources and Traditional Cultural Expressions, was drafted in Kenya in response to a growing need to address three main challenges facing the country: accelerating technological development, integration of the world economic, ecological, cultural, trading and information systems and the growing relevance of intellectual property rights to these areas of activity. The policy further sought to protect the owners of indigenous knowledge from being exploited through biopiracy and how accruing benefits could be shared amongst stakeholders involved. p) In 2011, World Bank survey estimated that there were potential 40,000 herbalists in Kenya compared to about 4, 500 conventional doctors. This presented and further revealed a very important human resources (health personnel) already existing in Kenya and whose shortage remains the biggest problem facing the national healthcare sector today as was noted by Dr Alfred Karagu, the then acting Chief Executive Officer at the Ministry’s National Cancer Institute (NCI). q) In 2014, WHO Traditional medicine strategy 2002-2005 was updated as WHO Traditional Medicine Strategy 2014-2023 to help healthcare leaders to develop solutions that contribute to a broader vision of improved health and patient autonomy. The strategy has two key goals: to support Member States (Kenya included) in harnessing the potential contribution of Traditional Medicine/Complementary/Alternative Medicine (TM/C/AM) to health, wellness and people-centred healthcare and to promote the safe and effective use of TM/C/AM through the regulation of products, practices and practitioners. r) Witchcraft Act (Cap. 67) that came into force on 12th November, 1925, Industrial Property Act No. 3 of 2001, The Copyright Act, 2001 (Chapter 130, 2014 Revised Edition), The Protection of Traditional Knowledge and Cultural Expressions Act 2016, and The Health Act 2017 ushered in the use and application of ethnomedicines alongside conventional medicine in Kenya. This Health Act of Kenyan Parliament for the first time legally brings Traditional Medicine/Complementary/Alternative Medicine (TM/C/AM) and ethnopractices fully under the national Ministry of Health alongside conventional medicine. While the bending private Bill at the National Assembly (Kenyan National Parliament), The Traditional Health Practitioners Bill, 20l4, sponsored by Member of Parliament, Rachel Nyamai and another similar Bill, The Traditional Herbal Medicine and Medicinal Plants Bill, 2014, sponsored by the Ministry of Health, once debated and passed, will contribute a great deal to the use, control, management and practice of ethnomedicines in Kenya. It therefore follows with logical necessity that in Kenya, the legal framework of TM/C/AM is gradually taking shape in time and space albeit its state of confusion/competition and resistance from the conventional practitioners. s) In 2017, the 2017-2022 Cancer Strategy launched indicated to educate its health workers and communities on the use and application of ethnomedicines for cancer treatment, control and management. t) These major developments from 2014 through 2015 and 2016 to 2017 culminated in efforts suggested way back in 2002 by the then Minister for Health, Prof. Sam Ongeri; to incorporate ethnomedicines at all levels of Kenya’s healthcare system in order to achieve “Health for All” but this was then strongly opposed by conventional doctors in Kenya, particularly the Kenya Medical Association.
u) In February 2017, during the 7th Kenya Medical Research Institute (KEMRI) Annual Scientific and Health Conference, evidence was presented supporting the use of some more than 20 locally available herbs in treating cancer. v) On Thursday, November 23rd, 2017 Maasai Mara University launched the tree planting exercise of medicinal plant species in its newly established, African Medicinal Botanical Garden (AMBG) at its Main Campus. The AMBG is to serve as one of the main ex-situ and in-situ conservation site in Kenya, as a resource centre for medicinal plants for study, research, consultancy and production. Additionally, this is part of the government’s strategy to combat desertification and increase the county’s forest cover and push it to 10 per cent by 2020. w) On Friday, December 1st, 2017, Maasai Mara University in partnership with the Wuhan Botanical Garden (WBG) of the Chinese Academy of Sciences (CAS) and in collaboration with Sino- Africa Joint Research Centre (SAJOREC), invited His Excellence, the Deputy President of the Republic of Kenya, William Samoei Ruto to commission the established African Medicinal Botanical Garden (AMBG). x) On 15th February, 2018, during the 8th KEMRI Annual Scientific and Health Conference with the Theme: Health Research for sustainable Development held between 14th and 16th February, 2018 at Safari Park Hotel, Nairobi, Kenya, KEMRI’s Traditional Medicines and Drugs Research Centre (TMDRC) organized a special symposium to address the state and way forward of Traditional Medicine/Complementary/Alternative Medicine (TM/C/AM) in Kenya.
y) On 31st August, 2018 and following the endorsement of the plan of action for implementation of the Decade of African Traditional Medicine declared in Lusaka in July 2001 and the institution of the African Traditional Medicine Day in Member States to be celebrated every year on 31st August with effect from 2003, Maasai Mara University organized for the National celebrations of the African Traditional Medicine Day.
z) On Wednesday, May 22nd, 2019 Maasai Mara University launched the Kenya Defence Forces (KDF) tree planting exercise of mainly medicinal plant species in its newly established, African Medicinal Botanical Garden (AMBG) at its Main Campus. The AMBG is to serve as one of the main ex-situ and in-situ conservation site in Kenya, as a resource centre for medicinal plants for study, research, consultancy and production. Additionally, this is part of the government’s strategy to combat desertification and increase the county’s forest cover and push it to 10 per cent by 2020.
As much as the three Acts mentioned in i) above need to be put into practice as the debate at the National Assembly awaits The Traditional Health Practitioners Bill, 20l4, and The Traditional Herbal Medicine and Medicinal Plants Bill, 2014, care need to be exercised in order to avoid contradictions and duplication of functions, operations, powers and authority of the various Acts involved in fostering appropriate integration, regulation and supervision at all levels, particularly the regulation of the capacity building, research, products and practice of ethnomedicines as well as ethnopractitioners
Great Challenges with Ethnomedicines: Public Health Concerns and Required Concerted Efforts
The use of modern science and/or conventional knowledge to measure ethnomedicines as an independent and unique system and two, the failure of conventional medical practitioners to fully recognize and accept ethnomedicines in the healthcare system, pose great challenges on how to alleviate the mistrust that has endured for ages. Restoration of confidence in an ethnomedicinal system labelled as satanic, witchcraft, myth, quack, evil, apprehensive etc, requires concerted efforts at all levels, providing evidence-based knowledge in public domain. Growing use and application of ethnomedicines and their market expansion pose challenges on safety, quality and efficacy of traditional remedies, notably assessment of products and services, qualification of ethnopractitioners, methodology and criteria for evaluating efficacy, which is unique to Traditional and Complementary Medicine (T&CM) and ethnopractitioners. Contaminated an adulterated products are common in ethnomedicine industry and reports of T&CM–based toxicities are also alarming in public [92]. Continued use and application of endangered species such as Slow loris and Shark fins in ethnomedicines without precautions and proper guidelines endanger and threaten the long-term survival of ethnomedicine industry. There is need for the development of the ethnopharmaceutical production policy and regulations governing chain supply strategies of the ethnomedicine industry. This has to be supported by the political will to provide the enabling environment for working and implementation of the Acts. The effect of poisonous ethnomedical resources and use of human as the guinea pig in the “laboratory” is really a worrying factor! The maintenance of a working relationship between ethnopractitioners, conventional practitioners and the industry/academia is indeed challenging. Similarly, the sustainable integration of T&CM into conventional healthcare system and scaling to cover primary, communal and national levels is just an uphill task, in particular identifying and evaluating strategies and criteria for integrating T&CM into national health and primary healthcare (PHC) systems. Lack of development of national policies to guide the sustainable utilization, protection, conservation and preservation of ethnomedical resources: plants, animals, soils and microorganisms versus nature conservation. Limited national organizational arrangements for institutionalization of Traditional and Complementary Medicine. Lack of insurance cover of those patients seeking health services of T&CM. Capacity building in Traditional and Complementary Medicine: what levels and how should the curriculum be developed, controlled and regulated, and by who? In Kenya, the law under development is however silent on this particular aspect, thus presenting a dilemma and creating loopholes that may be used unprofessionally. There is need to develop concerted efforts to address the issues of Intellectual Property Rights (IPR) of ethnoknowledge systems, equitable sharing of accruing benefits following commercialization of T&CM, bioprospecting and biopiracy at local, national and international levels. There is also need to ensure the availability of relevant information, enhancing access and promoting rational and international use and application of Traditional and Complementary Medicine
Which Way Forward for Ethnomedicines? The Recognition of Ethnopractitioners And Continuum of Togetherness.
Dreaming big to improve livelihoods in the society as we all read from the same script without mischief! Recognizing the fact that ethnopractitioners, conventional practitioners and industry, research institutions and academia are all equal partners, collaborators and/or players in health industry in Kenya. As a matter of facts, the three partners/collaborators/players must agree that globally, they are co-existing, competing, communicating, coordinating, collaborating and cooperating in their own unique ways of embracing survivalihood and henceforth, continued evolution of life that is optimally taken care of. Upon this realization, the three partners/collaborators/players should therefore come together to develop concrete, attainable goals and objectives with shared vision and the unique purpose of co-existence. The relationships for engagement should focus on a 3C framework of embracing coordinative, collaborative and cooperative in order to realize the unique purpose of co-existence in the health industry. The collaborative arm will ensure that the three partners are all equally involved in a plan or activity work together in an organized way for effective results and mutual benefit, authority and accountability for success and sharing of resources and rewards. The cooperative arm will ensure working jointly with others or together especially in an intellectual endeavor for effective results. While the coordinative arm will ensure that the three partners are working together to create or achieve the same thing. All these levels of engagements will improve the weaknesses of the three partners a great deal while building their strengths to greater heights as they grow and develop a healthy society [93-96].
I. The suggested continuum of togetherness should be able to: 1. Develop a robust and sustainable strategic mechanism of sensitization of the ethnomedicines at all levels in the local and native communities. 2. Provide a harmonious working relationship between ethnopractitioners and conventional practitioners with a view to institutionalizing traditional medicines in healthcare systems, jointly developing sustainable policies and products for implementation and unbiased regulatory mechanisms. 3. Initiate ethnomedicines research and development agenda involving ethnopractitioners, conventional practitioners and industry, research institutions, industry and academia to help provide scientific evidence on safety, efficacy and quality of ethnomedicines where necessary as observed during the Ministerial Conference on Research for Health in the African Region, held in Algiers, Algeria, from 23rd to 26th June, 2008 and adopted as the Algiers Declaration, 2008. 4. Initiate a regulated and controlled capacity building framework at all levels, including refresher courses for leading ethnopractitioners, Professional Certificate, Diploma, Undergraduate Degree programmes, master’s degree and Doctoral Degrees. However, integrate WHO-based training tools in traditional medicines and Primary Healthcare (PHC) to the training programmes, syllabi and curricula.
5. Renew the lost glory in traditional medicines by recognizing ethnopractioners as equal partners through a well-structured institutional-based policy document on Intellectual Property Rights (IPR) to protect the interest of the indigenous communities and its ethnopractitioners and taking into account fair and equitable sharing of benefits of relevant holders, in collaboration with relevant partners with regard to WIPO requirements in Geneva and as per the multilateral treaty, Convention on Biological Diversity (CBD) signed by 150 government leaders at the 1992 Rio Earth Summit. The Convention on Biological Diversity is an international legally binding treaty with three main goals: conservation of biodiversity; sustainable use of biodiversity; fair and equitable sharing of the benefits arising from the use of genetic resources. The WHO guidelines and regulatory frameworks for the protection of traditional medical knowledge and access to biological resources to their specific situations can therefore be guaranteed.
6. Initiate the formation of a regulatory National Board for Traditional Medicines, which will regulate and control the practice of traditional medicines, ethnomedical resources and capacity building at all levels including, refresher workshop- based training programmes for leading ethnopractitioners, Professional Certificates, Diploma, Undergraduate Degrees, master’s degrees and Doctoral Degrees. Will focus on capacity building skills in problem solving, communication, synthesis of information and working ability. 7. Promote collaboration and partnership amongst the three partners and play a key role in allocating and mobilizing adequate resources and strengthening capacity-building. 8. Harmonize the relevant sections of The Protection of Traditional Knowledge and Cultural Expressions Act, 2016 and Health Act 2017 together with that of the bending Bills at the Kenyan National Parliament, The Traditional Health Practitioners Bill, 20l4 and The Traditional Herbal Medicine and Medicinal Plants Bill, 2014, into one formidable Act that addresses all aspects surrounding ethnomedicine industry in Kenya.
9. An all-inclusive national taskforce with clear terms of reference need to be set up, with leadership preferably from the academia (because of its robust constitutional mandates on capacity building, research, community outreach and consultancy) so that a concept is drafted for discussion with the parliamentary committee in-charge of health in preparation for the development of a Bill to be tabled on the floor of the Parliament for debate and subsequent development into Act. 10. Promote interdisciplinary systems such as Traditional and Complementary Medicine to work in integrated approach to generate solutions to complex, dynamic societal problems, manage adoptively and inform decision-making processes. 11. Enhance resource mobilization, wealth creation and improvement of the livelihoods of marginalized communities identified to be the custodians of the indigenous knowledge, Traditional and Complementary Medicine and ethnopractices faced with either exploitation and/or extinction.
Anticipated Benefits Accruing from the Envisioned Continuum of Togetherness
Recognizing ethnomedicines as having a wide variety of therapies and practices and as one of the resources of primary healthcare services familiar to many people in the world, its growth and development through partnership and collaboration of ethnopractitioners, conventional practitioners and industry, research institutions and academia as equal partners in the health industry will result into a lot of benefits as follows:
i. Improved health and livelihoods in the society due to increased availability, accessibility and affordability of healthcare services. ii. Quality training/teaching of students, this is good for society. iii. Increase in business and profit-making for involved partners. iv. Increase in amount of research for partner institutions. v. Sustainable utilization of natural resources and conservation strategies. vi. Improved health industry at all levels. vii. Increased employment opportunities. viii. Ranking of institutions involved improves nationally and internationally. ix. The interaction makes staff improve in competencies. x. Increase in research output in form of products, publications and patents etc. xi. Pooling resources and individual strength together for a common goal xii. Increased and improved commercialization of knowledge xiii. Joint sourcing of research funds: easy to get! xiv. Sharing of research facilities and rewards.
The Case of Maasai Mara University in Narok County,Kenya
Maasai Mara University has partnered with The Wuhan Botanical Garden (WBG) of the Chinese Academy of Sciences (CAS), and in collaboration with Sino-Africa Joint Research Centre (SAJOREC) to establish an African Medicinal Botanical Garden (AMBG) at the Main Campus of the University. This idea of collaboration of a Chinese- aided China-Africa Joint Research Centre in Kenya, where African and Chinese researchers would conduct joint research, was conceived during deliberations between Prof. Robert W. Gituru of Jomo Kenyatta University of Agriculture and Technology (JKUAT) and his Chinese research counterpart, Prof. Wang Qing Feng, in 1999. Ever since its establishment, the Sino-Kenya ties has yielded a lot of fruits, among them, the ‘Sino-Kenyan Scientists’ Workshops’, the JKUAT Botanical Garden, training sessions for African stakeholders to various Universities and research institutes in China, scholarships for Kenyan students to the prestigious University of Chinese Academy of Sciences, and the on-going work of African Medicinal Botanical Garden of Maasai Mara University, Narok County.
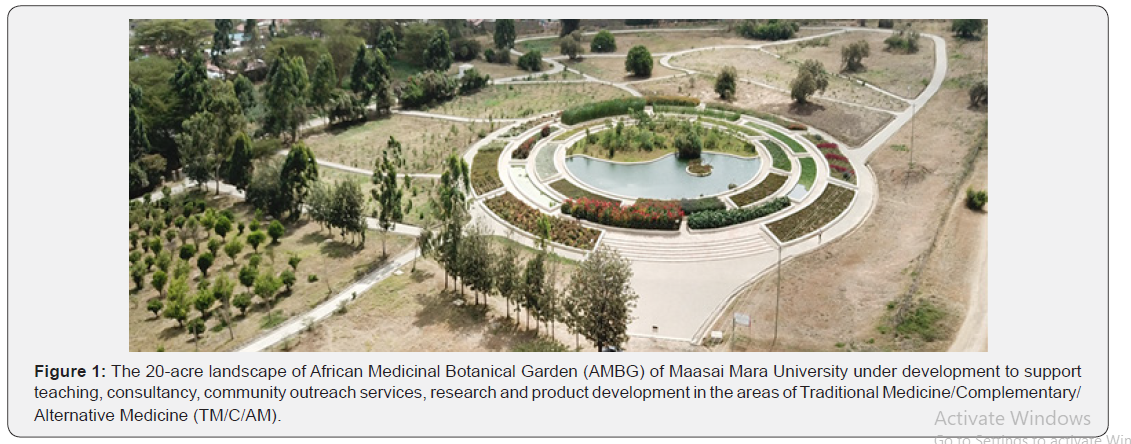
The University is developing the African Medicinal Botanical Garden on a 20-acre land to support teaching, consultancy, community outreach services, research and product development in the areas of Traditional Medicine/Complementary/Alternative Medicine (TM/C/AM) (Figure 1). The AMBG will serve as one of the main ex-situ conservation sites in Kenya, as an ethnobotanical and ethnomedicine resource centre for study, research, product development and consultancy, and as a centre for information dissemination on ethnobotanicals, ethnomedicines as well as general ethnoknowledge. The project commenced by planting a few available medicinal plant species (1053 seedlings comprising 67 species) from the nurseries of trees of Kenya Forestry Research Institute (KEFRI) headquarters and elsewhere in its branches during any rain seasons. Additional planting took place with medicinal plant species, which were raised in a plant nursery established at the University’s Main Campus, Narok County following capacity building of the University’s staff.
Careful observation of Figure 1 indicates that the area is a semi-arid one, therefore implying that the area has limited amount of water supply and/or availability. The University therefore innovatively devised a technology of cleaning wastewater using a biological means, which is Common Water Hyacinth plants filtering system. Semi-cleaned wastewater from the sewage is pumped into a series of joined compartments, each filled with the Common Water Hyacinth plants for further purification before it is released in the field for watering plants at various designated water points. Meanwhile, in preparing to ensure that as a stakeholder institution, Traditional and Complementary Medicine work in integrated approach, the University is keen at establishing the state-of-theart laboratories for teaching, research and product developmentIn addition, the University is planning to engage the local communities so as to partner and collaborate with them in research and product development in the areas of Traditional Medicine and capacity building.
Conclusion
It is important to fast track the organization and integration of ethnomedicines into the mainstream conventional healthcare systems at all levels and in line with the WHO guidelines and standards as outlined in its resolutions, declarations and strategies within the framework of the country’s constitution. For sustainable growth and development of Traditional Medicine/Complementary/ Alternative Medicine in Kenya, the two Acts and the two Bills yet to be tabled in the National Assembly, there is need to be harmonized them into one formidable Act through a national task force, preferably led by the academia for its strong constitutional mandates on capacity building, research, consultancy, community outreach services and policy formulation. In this Act, clarity on control and regulation of capacity building, research, practice, Intellectual Property Rights (IPRs), well defined functions, powers and authority of the Council/Board, mandates of operating committees and sub-committees, and consultation and inclusivity amongst concerned stakeholders should not be ignored. It should be noted further that IPRs are protected in law by, for example, patents, industrial designs, copyright, geographical indications and trademarks to help foster a culture in which innovation and creativity are celebrated, protected and enable people to earn recognition or financial benefit from what they invent or create.
Acknowledgements
We are very grateful to the Wuhan Botanical Garden (WBG) of the Chinese Academy of Sciences (CAS), and Sino-Africa Joint Research Centre (SAJOREC) to partner and collaborate in establishing an African Medicinal Botanical Garden (AMBG) at the Main Campus of Maasai Mara University. We are also thankful to the organizers of the 8th KEMRI Annual Scientific and Health Conference with the Theme: Health Research for sustainable Development held between 14th and 16th February, 2018 at Safari Park Hotel, Nairobi, Kenya, where this manuscript was first presented and critiqued by colleagues during the KEMRI’s Traditional Medicines and Drugs Research Centre (TMDRC) organized symposium to address the state and way forward of Traditional Medicine/Complementary/Alternative Medicine (TM/C/AM) in Kenya. To them all we are very grateful.
For more Open access journals please visit our site: Juniper Publishers
For more articles please click on Journal of Complementary Medicine & Alternative Healthcare




Comments
Post a Comment