Comparison of Analgesic Efficacy of Paracetamol and Pethidine for Pain Relief in Active Labor-Juniper Publishers
Juniper Publishers
Abstract
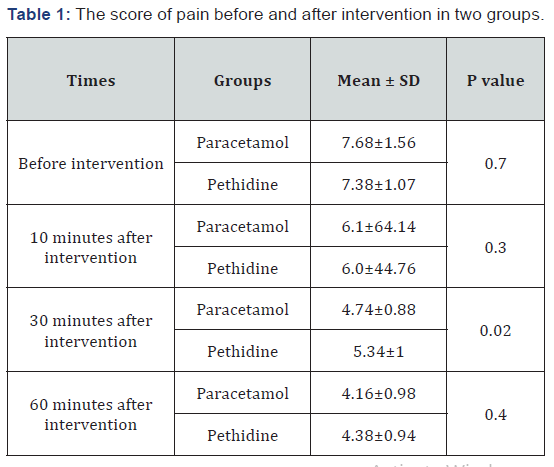
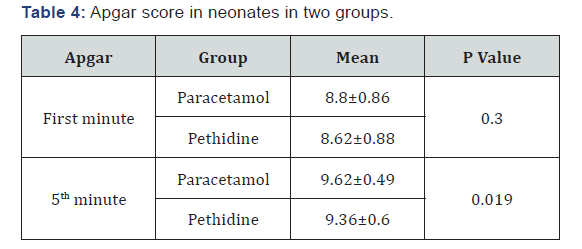
Background and Objective: Using pain-relieving drugs during labor is now part of standard care in many countries throughout the world. There are many methods for reducing pain in labor time and each method has its own risks and benefits. The aim of this study was to assess the efficacy of pethidine versus paracetamol as an analgesic during labor in pregnant women. Methods: In this clinical trial study, 100 women expected to have a natural childbirth were observed and then randomly allocated two groups. The first groups receive paracetamol and the second group receives pethidine. The intensity of labor pain experienced by the subjects and the outcome of delivery were collected by a checklist. Results: There was a significant difference between the average pain score in paracetamol and pethidine groups in 30 minutes after intervention, but there was not a significant difference between the severity of the pain in two groups before intervention and 10 and 60min after intervention. No significant differences were seen regarding duration and interval of uterine contractions, neonatal complications, first minute Apgar score and side effects of used drugs between the two studied groups. There was a significant difference between the average of fifth minute Apgar score and mother SBP and RR after intervention between two groups. Conclusions: Use of paracetamol reduces pain more than pethidine within 30 minutes after intervention
Keywords: Pethidine; Labor pain; Paracetamol; Ardabil
Introduction
Today pain is one of the major causes that caused pregnant women don’t tend to have normal delivery. Pain relief is a major part of the science of midwifery. Severe labor pain is associated with psychological and physiological complications on mother and fetus. Labor pain and its prolonged duration are the most important factors in encouraging pregnant women to cesarean delivery which not only requires more specialized facilities and higher costs, it also causes more maternal complications. Therefore, reducing labor pain and its duration is one of the major steps in reducing misplaced cesarean delivery [1-2]. Labor pain is one of the most severe pain experienced by women during their lifetime [3]. This pain is especially severe and longer in primiparous women [4]. The cause of labor pain is cervical stretching during dilatation and ischemia of the uterine wall during lactate production [3]. Pain is an unpleasant feeling that medical science has always been trying to eliminate or reduce it [6]. But, the severity and extent of pain tolerance vary in individuals and under different conditions [7-8]. Based on studies, 77% of primiparous women described labor pain as severe and intolerable [9]. Labor pain can have many adverse effects on delivery process, maternal and fetal status [10]. Severe labor pain may cause long-term imbalances that disturb the mental health of the mother and has a negative effect on the relationship between mother and baby in the first days of life which was very important [11]. Unwanted side effects due to labor pain in the fetus including late loss of fetal heart rate following the reduction of maternal arterial oxygen pressure, decreased uterine patchy blood flow due to severe uterine contraction during labor pain and fetal acidosis, which occurs in some cases [12]. According to studies, today most of women want a form of analgesia at the time of delivery [13]. For more reasons there is no way to relieve labor pain in Iran and so evaluation cheap and safe methods in this field is necessary. Various methods have been proposed for the relief of labor pain, among which non-pharmaceutical methods can be mentioned which their most important advantage is that they are uncomplicated and that their greatest defect is low effect [1]. Nonpharmacological methods included physiological delivery, delivery in water, maternal delivery in the presence of the spouse, relaxation, hypnosis, aromatic therapy and electrical stimulation. But due to the convenience and the most commonly used pharmaceutical methods, includes epidural anesthesia, spinal anesthesia, injection of sedative and opiate drugs and the use of gases such as antonox have been used for the relief of labor pain.
Today there are many methods and medications that reduce or reduce the severity of labor pain [14]. These methods are divided into four groups of psychological methods, pharmacological methods, local anesthetics and inhalation anesthetics [15]. It seems pethidine can accelerate labor by reducing maternal concentrations of catecholamines in some patients [16-17]. Pethidine is a narcotic drug that is produced by the industrial method and used to treat moderate to severe pain. In the twentieth century, pethidine was one of the most popular opioids both for acute and chronic pain. This drug in the United States is known with name meperidine [18]. Paracetamol (acetaminophen, N-acetyl-P-aminophenol) is a non-opioid analgesic that was marketed in 2002 as an intravenous infusion vial called Perforlgan. Paracetamol is an effective and safe drug with known analgesic effects, which has fewer side effects than meperidine [19]. This drug is available in Iran with the apoutel brand name in the form of 1000mg vials. The onset of the analgesic effect is 5 to 10 minutes and the maximum effect time is one hour and the duration of the effect is 6-8 hours [20]. Paracetamol is a good remedy for mild and severe pain [21-22]. Some studies have found that analgesic effects of paracetamol in reducing pain are better than meperidine [23]. Considering the increase in cesarean section rate and the promotion of normal delivery, this study aimed to compare the efficacy of paracetamol and pethidine in reducing labor pain.
Methods
This was a randomized double blind study (Randomized clinical trial) that has been done on 100 pregnant women in the first and second parity referred to the Ardabil Alavi hospital in the active phase of labor. This study was double blind and the division of patients and injections was done by blinded persons. In this study among pregnant women who were referred to Alavi hospital in Ardabil 100 pregnant women were selected and they were randomly to groups A and B. Group A (50 cases) was injected with intravenous paracetamol at a dose of 1g and placebo and group B (50 cases) received intramuscular injection of pethidine 50mg and placebo intravenous injection. Pregnant women with singleton (37-41 weeks)-start of active phase of labor- Cephalic presentation-no fever or serious systemic illness-lack of fetal distress-lack of meconium-the lack of coagulation disorders were included in the study. Patients underwent pulsed oximetry and continuous monitoring of FHR. The checklist included age, weight, obstetric records of the pregnant mother, type of analgesia, fetal heart rate, active phase of labor, duration and intervals of uterine contractions, Apgar score in the first and fifth minutes, pain scores before and after analgesia and complications for women have been completed. Significant symptoms of the patients (blood pressure, heart rate and respiratory rate before and after pain) recorded and pain scores based on VAS were measured in minutes 10, 30 and 60. Pregnant women with disorder in fetus FHR, lack of progress in delivery, macrosomi, vaginal delivery and response to these drugs were excluded from the study. This study was approved by the University’s Ethics Committee with the IR.ARUMS. REC.1396.202 number and registered in the Iran clinical trial database by code IRCT20150808023559N17. The collected data were analyzed using descriptive statistical methods such as tables, figures and statistical indices as average and standard deviations and statistical analytical methods in the form of various statistical tests to compare the relationship between quantitative and qualitative variables in the spss version 19. The p<0.05 was considered significant.
Results
The average age of patients in the paracetamol group was 23.44±7.73 and in the pethidine, group was 24.98±5.15 and the difference wasn’t significant. Most of women were in age group 21-30 in both groups. The mean of gestational age in paracetamol group was 38.8±2.92 and in pethidine group was 38.7±1.3 weeks and there was no significant difference between the two groups. The average score of pain in the patients in the paracetamol group was 7.68±1. 56 and in the pethidine, group was 7.38±1.97 and there was no significant difference between the two groups before the intervention
The average of pain intensity 10 minutes after the onset of the intervention in the group receiving paracetamol was 6.64 and, in the pethidine, group was 6.4 and there was no significant difference between the two groups Table 1.
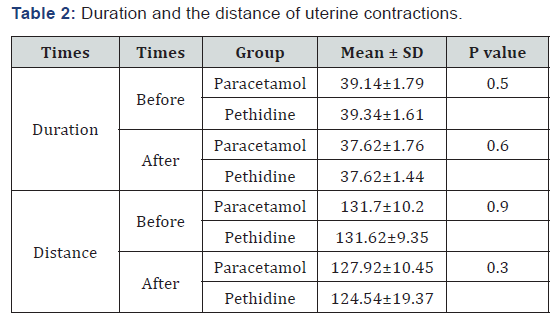
The mean of uterine antractions after using drug compare to before using drug in paracetamol group was 4.36±1.12 and in pethidine group was 4.04±0.98 and the difference wasn’t significant. The mean of duration and distance of uterine antractions after using drug in compare to before drug use wasn’t significant between two groups Table 2.
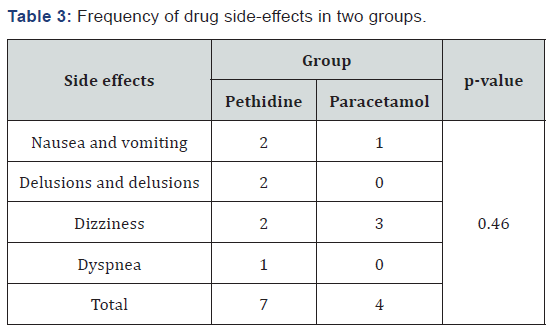
In study the side-effects of used drug it was leveled that except the nausea, vomiting and headache which was lower in the paracetamol group than in the pethidine group there was no significant difference between the two groups in other side-effects. The incidence of complications in the pethidine group with 7 cases was higher than paracetamol group with 4 cases Table 3. Base on the findings of the study, the first- and fifth-minute neonate Apgar score showed that the majority of newborns had fifth upgar score above 9. Apgar score was higher in the paracetamol group than pethidine group and there was no significant difference between two groups in the first minute but in the fifth minute this difference was significant Table 4.
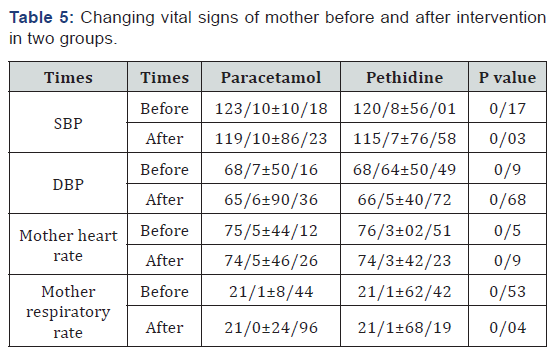
The number of heart rate of the fetus in the paracetamol group was 140.6±4.13 and in the pethidine group was 140.44±56.4 and there was no significant difference between the two groups. The mean of systolic blood pressure and maternal respiratory rate in the treatment groups were statistically significant in the post intervention period but there was no significant difference in heart rate and diastolic blood pressure Table 5.
Discussion
The results of this study showed that the degree of pain reduction based on VAS was lower in the drug receiving groups after administration of the drug. The degree of pain reduction in the group receiving paracetamol 30 minutes after receiving drug was significantly less than pethidine group. But, over time with the absorption of pethidine the average of the numerical scale was not statistically significant for 60 minutes after intervention in the treatment groups. Allameh in a study that evaluated the effects of pethidine during delivery concluded that pain score 30 minutes after intervention was 7.8 in the control group and 6.87 in the treatment group [24]. In this study this number was 5.34 which was lower than Allameh study, stated that pethidine has the greatest effect on end stage delivery (Cervical dilatation is more than 3 to 7cm) and this would also have the least effect on maternal and fetal health [25]. In the study it was concluded that paracetamol leads to a reduction in pain score in patients [19]. In a study on patients with renal pain intravenous paracetamol was a safe and effective drug for relieving pain in patients with renal pain which could produce an analgesic effect without significant complications. Also, the results showed that paracetamol has a higher efficacy and fewer side effects than tramadol in reducing pain in patients with renal pain [26]. In a study comparing paracetamol and morphine to postoperative analgesia it was concluded that paracetamol can be used as an alternative to morphine to induce analgesia after surgery with moderate pain. Although the researchers noted that morphine produced a better short-term analgesic effect and finally the effect of paracetamol remains longer [27]. In the study of Abdollahi paracetamol produced a better analgesic effect than pethidine which is consistent with our study [28]. It seems pethidine in some patients may reduce the maternal concentration of catecholamines in the bloodstream which can accelerate the delivery [17].
But there was no significant difference between the two groups in terms of duration and contractions. The average systolic blood pressure and maternal respiratory rate after drug use were significantly different between the two groups. But the average of mother diastolic blood pressure and heart rate after drug were not significantly different between the two groups. Findings of the study on the first and fifth minute neonatal apgar showed that the majority of newborns with the first minute Apgar score above the eight and fifth grade upgrades were above nine and there was no statistically significant difference between the two groups in the first minute after delivery but the difference was statistically significant in the Apgar score in 5th minute and in the paracetamol group was more . Apgar score was higher than 8 in minutes 1 and 5 which is in line with the results of this study [28]. There was no significant difference in terms of uterine contractions and the interval between them after drug use between the two groups. In Johnter’s research using internal monitoring it was found that pethidine increases intrauterine pressure and the severity of uterine contractions while the duration and distance of the contractions do not change [29]. Kamyabi don’t observed different in the number and intervals of uterine contractions in the pethidine and control group which was in line with the results of the present study [30]. Studies have shown that taking pethidine at doses less than 100mg does not cause fetal complications during delivery and if the baby is born within one to four hours after taking pethidine, the probability of a baby’s depression is low [17]. In the pethidine at dose 75mg did not have any side effects for the mother and no difference were found in blood pressure, heart rate, maternal respiratory rate and heart rate of the fetus before and after the injection [30]. Neonates born in both groups had a good Apgar score and none of the babies needed naloxone administration and resuscitation [30]. The results of this clinical trial were similar to the study of Mesadegh zadeh and Hontosh zadeh [31-32]. In the study there was no difference between the two groups of paracetamol and pethidine in terms of drug side effects [28] which was in line with the results of this study.
Conclusion
Using paracetamol reduces pain more than petidine within 30 minutes after taking the drug. Using paracetamol has less side effects on mothers than pethidine. Neonates born to mothers of parestamol group had higher Apgar scores compared to those born to mothers of pethidine group.
For more Open access journals please visit our site: Juniper Publishers
For more Open access journals please visit our site: Juniper Publishers




Comments
Post a Comment