Novel Integrated Approaches for the Detection and Management of Type-2 Diabetes- juniper Publishers
Juniper Publishers- Journal of complementary medicine
Abstract
Global Burden of Disease (GBD) Group, has published a
series of articles in the reputed journal of Lancet, in the last few
years providing the readers, access to vast amount of statistical data,
on the rapidly increasing Global Burden of Diseases across the Globe. In
the area of cardiometabolic diseases, they report that all the known
metabolic diseases, such as hypertension, excess weight, obesity,
prediabetes, diabetes (type-2), and vascular diseases, have reached
epidemic proportions. In spite of these observations and innumerable
reports, hardly there is any major report, suggesting ways to stop,
reduce, reverse, or prevent these chronic diseases. If these diseases
are not checked in the near future, the economic disaster they cause,
will be disastrous for the developing nations, which carry the major
healthcare burden of these diseases. Framingham Heart Study group, which
was initiated 70 years ago, by the prestigious National Institutes of
Health (NIH) USA, developed a list of modifiable risks, that promote
cardiovascular diseases. Several studies since then, have shown that
managements of these modifiable risks, have contributed significantly,
to the decline in deaths due to CVDs worldwide. However, there is no
such clear-cut risk factors described, for other metabolic diseases. In
view of this fact, no country has reduced, or reversed, the rate of
increase of metabolic diseases in the last three decades. Since this
article is about diabetes, we will focus on this particular disease and
discuss our options to contain this disease. In majority of the
countries, standard diabetes care seems to be, treatment of patients,
with oral hypoglycemics, and then follow with insulin therapy, when oral
medications fail or become inadequate. We will discuss in this
overview, early risk factors for the development of metabolic diseases,
starting from the time of conception, and available options for
interventions. We also will discuss childhood obesity, oxidative stress,
inflammation, endothelial dysfunction, and subclinical atherosclerosis,
as possible causes of observed metabolic risks, and suggest
complimentary therapies, for these observed risks. Finally, using India
as a model for the developing countries, we will suggest a few options
for implementing, population-based prevention strategies.
Keywords: Global burden of disease; Cardiometabolic diseases; Metabolic diseases; Hypertension; Diabetes
Introduction
In the last three decades there is a rapid increase
in cardiometabolic diseases such as hypertension, excess weight,
obesity, type-2 diabetes and vascular diseases to epidemic proportions
worldwide [1-13]. In the same period the incidence of type-2 diabetes
has increased over 17-fold in China [14]. By and large, the reason for
this global increase seems to be the rapid urbanization, ease in
commuting, sedentary habits, unhealthy lifestyles and Western diet
pattern. In view of this observation, there has been some attempts to
initiate, global prevention strategies. With this goal in mind, United
Nations General Assembly in October of 2018, during the Plenary Meetings
of the Seventy-Third Session, adopted two resolutions, -General
Assembly Reaffirms Political Declarations on Urgent Global Responses to
Tuberculosis, Non-Communicable Diseases (NCDs). The assembly adapted the
resolution, “political declaration of the third high-level meeting of
the General Assembly on the prevention of non-communicable diseases.”
This declaration is nothing but the re-adaptation of the earlier
declarations,
which all member countries had signed. The representative of Italy,
explaining her delegation’s position said, that she had the honor to
co-facilitate negotiation and that the declaration is concise, balanced,
and builds on current opportunities. The resolution highlights the
importance of healthy lifestyle choice for the prevention of
non-communicable diseases. The high-level committee “Approved Draft
Declaration, World Leaders in General Assembly Pledged Increasing Multi
Stakeholder, Multisectoral Response to Tackle Non-Communicable
Diseases.”
In a historic United Nations’ (UNs) Summit on
September 25, 2015, the world leaders adopted the 17 Sustainable
Development Goals (SDGs) to be achieved by 2030. Three interconnected,
core elements, namely economic growth, social inclusion, and
environmental protection, are identified for sustainable and inclusive
growth of all. In the past few decades, noncommunicable diseases (NCDs),
have emerged as a major public health problem in the world, due to
demographic, epidemiological, and socioeconomic transition. Recognizing
the social, economic and public health impact of NCDs, the WHO
Global NCD Action Plan 2013-2020 and nine voluntaries global
NCD targets were adopted by the World Health Assembly in 2013.
This document provides information about the voluntary global
target, to halt the rise in diabetes by 2025. Reaching this target is
also an important step, toward realizing the commitments made
at the UN General Assembly High-level Meetings on NCDs in 2011
and 2014, and the vision of the 2030 Agenda, for Sustainable
Development and the Sustainable Development Goals (SDGs),
including target 3.4 to reduce premature NCD mortality [15,16].
Considering the progress made in the last five years, since the
adaptation of the SDG, the experts predict, that chances of
stopping the increase in the incidence of diabetes worldwide
by 2015, is less than 1 percent. According to the experts, over
415 million people live with diabetes and estimated 193 million
people have undiagnosed diabetes [17]. Early detection through
screening programmes and the availability of safe and effective
therapies, will reduce morbidity and mortality by preventing or
delaying diabetes-related complications.
Traditional Medicine practitioners of India and China have
used herbal medicine and various phytochemicals for centuries
and reaped the benefits of their medicinal properties. However,
the regulatory agencies of the US, the UK and EU will not allow
the sales of these drugs as therapeutics. In the USA, Public Health
Services established a National Center for Complementary and
Alternative Medicine (NCCAM) in 1991. Over 50 US academic
institutions, have complementary medicine programs funded
by NCCAM. Dr Josephine Briggs the ex-director of this Institute
says, “that the use of herbal medicine is not acceptable, as they
do not meet the safety and efficacy criteria established by the
US regulatory agencies (FDA). The name of this center has been
changed to National Center for Complementary and Integrative
Health (NCCIH). Now the question that rises in the minds of
those, who want to promote integrated health programs is, how
do we accomplish this goal without doing very expensive often
confusing and contradicting large clinical trials? Since 1980,
obesity has increased worldwide by two-fold and diabetes fourfold.
Patients with diabetes, have a two to three-fold higher risk for
developing cardiovascular disease and cerebrovascular diseases.
How did we reach this sorry state, in spite of the tremendous
improvements in health care worldwide? What other measures
should we take, to reduce or prevent these chronic metabolic
diseases? In this review, we will try to address some of the issues,
and discuss some alternative, or complementary approaches.
Since China and India, have highest number of subjects with
diabetes, we will use these countries as model countries, for the
development of an integrated approach, to the management of
diabetes.
Discussion
Healthcare workers all over the world, are aware of the
inadequacy of the western medicine, which is disease centric
and the merits of integrated approach to health. In recognition of
this awareness, National Insitutes of Health (NIH) USA dedicated
a separate Institute, to address issues related to complementary
and alternative medicine (CAM). However, the regulatory
agencies in the USA, the UK, and the European Union, have banned
the sales of herbal medicine in their respective countries, citing
safety and efficacy issues. In recognition of the growing body
of evidence about the importance of integrative approach to
health, in 2009 Institute of Medicine (IOM), NIH, USA, organized
a summit on Integrative Medicine and Health of the Public. More
than 600 health care providers participated in this summit. The
IOM summit summary states, “The disease-driven approach
to care has resulted in spiralling costs as well as a fragmented
health system, that is reactive and episodic, as well as inefficient
and impersonal.” In spite of these international efforts, no
country has developed an integrated, holistic approach, to the
management of cardiometabolic diseases, which have reached
epidemic proportions worldwide. As we have mentioned before,
western medicine is disease centric, as such has not been very
effective, in the development of holistic or integrative approach,
to the prevention of chronic diseases. On the other hand,
traditional medicine, which claims holistic practice of medicine,
is also competing for the same space, with allopathic clinicians
and as such, are missing a great opportunity for developing
robust preventive medicine approach for stopping, reducing,
reversing, or preventing cardiometabolic diseases.
In China and India over the last century, traditional medicine
has co-existed with allopathic medicine. There are 350,000 staff
working at more than 2500 hospitals of traditional medicine in
China. India has over 700,000 Ayurvedic practitioners, there is
one primary health care center (PHC) for every 30,000 population,
and 5 to 6 community health centers (CHCs) for each PHC. What
we are trying to propose is a bold novel approach, to integrate
some aspects of traditional medicine, with some allopathic
methods and come up with a robust, holistic, integrated platform
for the management of metabolic diseases. After all, the back
bone of the Indian and Tibetan Traditional medicine is, “Dosha
System of Classification of Altered Metabolism.” Therefore, this
approach provides a great opportunity, to put to test this ancient
concept, and develop holistic approaches, to the management of
chronic metabolic diseases [18,19]. When attempting to propose
such an approach, it is important to take into consideration the
existing infrastructure, human resources, and various state and
national level initiatives. We also have to consider, as to what is
the earliest metabolic alteration, that we need to address in this
holistic integrated approach. Both in India as well as in China,
there are some efforts to introduce health education in school
curriculum, to promote physical activity and health eating
habits. Complementary to this educational program for school
going children, another program to empower women should also
be initiated.
Published evidence shows, that 15 million of all deaths
attributed to NCDs, occur between the ages of 38 and 69 years.
Of these “premature” deaths, over 85% are estimated to occur, in
low-and middle-income countries. Both China and India, share a common origin of NCDs. It has been very well established by
decades of epidemiological studies, that more than 30% of the
children born in Asian countries, are of low birth weight. These
children are at risk, for developing cardiometabolic diseases,
at later stages of adult life [20,21]. Harvard researchers have
developed, multi nutrient supplements, to reduce this observed
health burden [22]. Ayush trained clinicians, should be able
to provide the needed consultations to “would be” parents,
about the importance of micronutrients, and also recommend
multinutrient supplements during this critical period in life, to
prevent the fetal origin of adult diseases [23].
Recently AYUSH, the platform that is responsible for
Traditional Medicine Education in India, announced “Ayush
Therapy” at Government Centers, for borderline lifestyle
ailments. All metabolic diseases, such as hypertension, excess
weight, obesity, prediabetes, diabetes, and vascular diseases, are
lifestyle diseases by definition. The type of program suggested
by the AYUSH, makes a great sense, and if implemented properly,
can revolutionize the way healthcare is provided in a country
like India. The program announced by AYUSH envisages,
establishment of this kind of therapy at the 201 NCD-centers
across the state. We would like to see such program established,
in all the 15, 2326 PHCs, in the 640 districts of the country.
Furthermore, we also advocate the use of modern diagnostic tools
and platforms, for the diagnosis of the various metabolic risks, so
that the therapy can be initiated at the appropriate stages and
the progression or regression of the risks managed properly. If
we take this approach of early detection of the various metabolic
risks, and management of observed risks, then we can hope to
achieve the containment, or reduction of metabolic diseases in
the near future.
Next level of the preventive strategy should be, to look at the
childhood obesity and prediabetes. The Asian phenotype has a
different kind of obesity compared to the Caucasians. Therefore,
looking at the body-mass index (BMI) may not be the ideal
approach. We have demonstrated in our earlier studies, that Waist/
Hip ratio will be a better approach to monitor abdominal obesity
than the BMI. At the same time, screening should be initiated to
look at the fasting glucose, as well as postprandial glucose, to
detect early onset of diabetes or pre-diabetic conditions. These
types of tests will help in identifying individuals with borderline
lifestyle disorders [24-26]. Detection at this stage in life,
will help prevent, further progression of the diseases, or at least
postpone the development of clinical complications. For the
diagnosis of blood glucose levels, any standard over the counter
glucose monitor may be sufficient. However, if the staff can be
trained to use the continuous glucose monitors (CGMs), available
in the market, such as Abbott FreeStyle Libre, or Dexcom G6,
then one can develop simple methods, to measure interstitial
glucose profiles, as well as to validate the efficacy or otherwise
of a variety of anti-diabetic indigenous medical preparations,
dietary components, and formulations. In a representative figure
shown below, you can see the fluctuations, in the interstitial
glucose levels over a period of 12hours. The glucose levels are
determined every fifteen minutes. In the Dexcom G6 device, the
glucose is monitored every five minutes. Since one can access the
data any time during study, one can follow the beneficial effect
of it or lack of it, of any phytochemical (Eg: mulberry green tea
or herbal products), or a variety of indigenous anti-diabetic
preparations, dietary or nutritional therapies (Figure 1).

Leading herbal product developer Himalayan Drugs,
of India, has an anti-diabetic drug called, Diabecon, which
contains ingredients from: Gymnema sylvestre, Pterocarpus
marsupium, Glycyrrhiza glabra, Casearia esculenta, Syzgmium
cumini, Asparagus racemosus, Boerhavia diffusa, Sphaeranthus
indicus, Tinsopora cordifolia, Swertia chirata, Tribulus terrestris,
Phyllanthus amarus, Gmelina arborea, Gossypium herbaceum,
Berberis aristat, Aloe vera, Triphala, Commiphora wightii,
shilajeet, Momordica charantia, Piper nigrum, Ocimum sanctum,
Abuilton indicum, Curcuma longa, Rumex maritimus. Whereas,
another product Diasulin contains; Cassia auriculata, Coccinia
indica, Curcuma longa, Embilica officianlis, Syzugium cumini, Trigonella foenum graecum, Azadrichta indica, Ficus racemosa,
Aegle marmelos, Cinnamomum tamala. Some Ayurvedic
products have Gurmar (Gymnema sylvestre) Karela (Momordica
charantia) Pushkarmool (Inula recemosa), Jamun gutli (Syzygium
cumini) Neem (Azardochta indica) Methika (Trigonella foenum
gracecum) Guduchhi (Tinospora cordifolia). The advantage of
using CGMs to monitor glucose profiles, is that one can follow
the effect of any of the complementary or alternate therapies, for
their supplementary effect, in addition to whatever therapy that
they may be taking for the management of diabetes. Using such
approach, we have done preliminary studies on mulberry green
tea, which had antiglycemic properties.
In countries like China and India, the growing prevalence
of maternal obesity, gestational obesity, childhood obesity,
and early onset diabetes and prediabetes, lead to premature
mortality and morbidity. Furthermore, in Asian phenotype,
central abdominal obesity as measured by waist circumference is
a strong predictor of diabetes. This visceral obesity is associated
with abnormal levels of adipokines, low grade inflammation, and
insulin resistance. Early- onset of diabetes, increases the risk of
premature mortality and diabetes-related complications, due
to long duration of the disease. In China, the Da Qing Diabetes
Prevention Program, demonstrated the benefits of lifestyle
modification, in reducing the risk of progression from impaired
glucose tolerance to diabetes. In 2010, the Ministry of Health
launched a comprehensive NCD prevention and control program,
including health education and promotion, early detection
and treatment, and standardized disease management at the
community level in 140 counties, in 30 provinces in China [27].
We would like to see a similar diabetes prevention program
developed in India, at the community level (PHCs/CHCs), using
trained healthcare workers, Ayush Vaidyas, and any other NGOs
interested in such prevention programs. Any population-based
prevention program, developed by India and China, with such
large prediabetic population, can be used as model for other
developing countries.
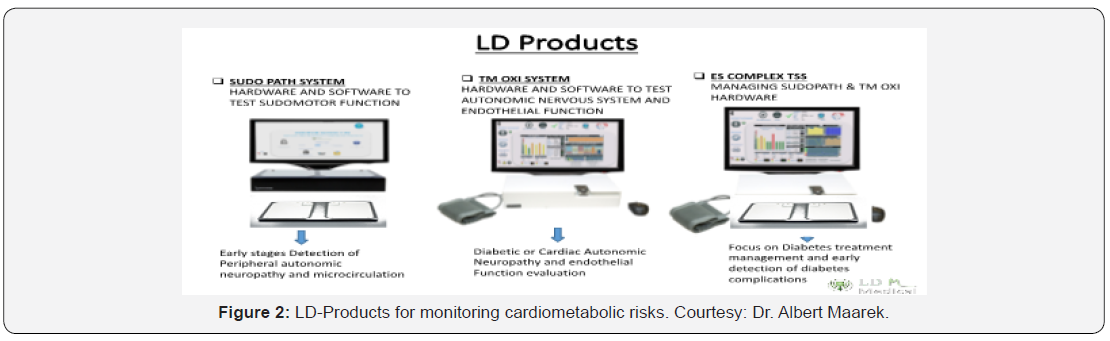
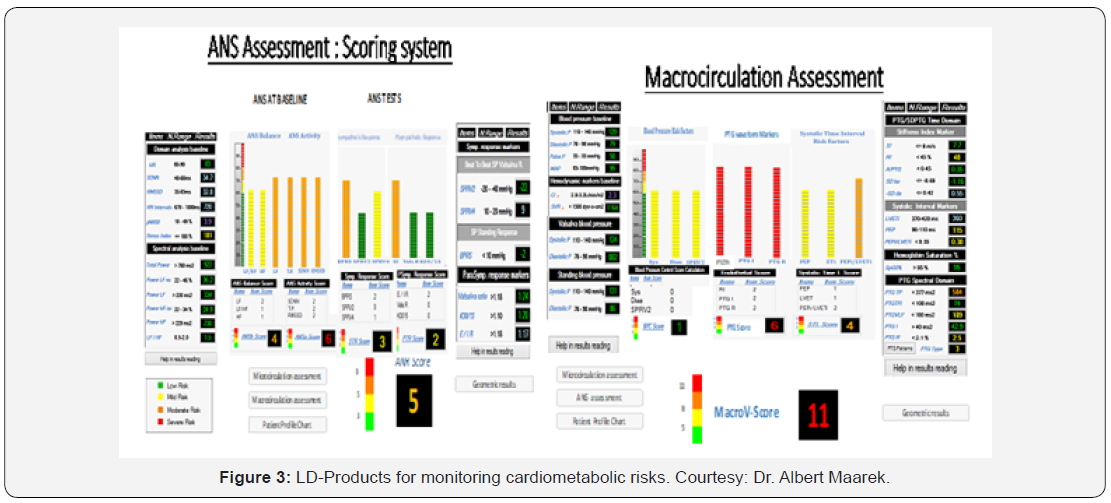
In this overview, we have discussed the benefits of using
CGMs for monitoring glucose profiles, as well as to evaluate the
effectiveness or otherwise of complementary therapies. We can
also add other noninvasive, simple to use diagnostic devices,
to this approach, for monitoring cardiometabolic diseases for
risk stratification, risk management, and prevention strategies
[28-31]. (LD-Products, Miami, Florida, USA: www.ldteck.com)
(Figure 2 & 3).
When planning a new novel and integrated approach to
healthcare, we need to consider the disparity between personal
choices, the differences that exist between the allopathic
doctors, and the traditional medicine Viadyas. At the time of this
writing, it is unthinkable that the West will accept traditional,
complementary and alternative medicine (TCAM). In one form
or the other, acupuncture, Ayurveda, Chinese medicine, are
popularized in developing countries today, and seem to enjoy
better attention, due to their popularity, integration, and holistic
approach to healthy life. In this article, our emphasis is more
on Integrative Medicine, than alternate or complementary
medicine. Integrated medicine, - refers to certain evidencebased
management, which uses best of both conventional and
traditional medicine systems. It is quite evident, that Western
medicine is disease centric, and has failed to prevent chronic
metabolic diseases. Traditional medicine is patient centric,
which claims to be holistic, yet, has failed to prevent the increase
in the evidence of metabolic diseases. The reason being, in
most of the developing countries, people do not go to seek
medical help, unless they are sick. How do we integrate these
systems, to achieve a balanced approach to health care, which
aims at arresting, reducing, or reversing the increase in the
incidence of metabolic diseases? It is important to ensure, that
the knowledge and training of TCAM practitioners are adequate.
It is also equally important, to develop a good understanding
between the TCAM practitioners, and the conventional medicine
practitioners, so that they understand the complementary nature
of the Integrative Medicine. This brings us to the immediate need
for change in the medical education system. In some countries
TCAM courses are integrated into allopathic medical education.
In others, the TCAM education also includes, teaching of some
common topics, essential for understanding the essence of
Integrated medicine.
According to experts in the area of TCAM, around 80% of
the population continues to use the traditional medicine in
Africa, Asia, and Latin America, and many governments in these
regions, have been trying to incorporate traditional medicine
practices, to help their primary health care needs. We have
already mentioned some of the efforts, under consideration, in
terms of diabetes education at various levels, development of
awareness programs, and encouragement of personal level as
well as population level prevention strategies. In view of the fact,
that we are advocating the development of Integrated Medicine
in developing countries, we also should emphasize the need for
the development of guidelines and guidance statements, that
would serve the needs of various healthcare providers. One size
fit all, approach will not work. Furthermore, these guidelines,
should be developed by the joint efforts of AYUSH experts and
the Medical Council of India experts, taking into consideration
that each group of practitioners, that is TCAM and allopathic,
blend seamlessly in terms of providing Integrated care for these
novel programs. These guidelines should consider, the need to
empower, and encourage, the TCAM practitioners, the use of
emerging tools and technologies, for diagnosis and management
of risks, as well as for monitoring benefits or otherwise of the
therapies. They should be made aware, that if the traditional
medicine approach fails, the subjects should be advised to
switch to conventional medicine therapies. Similarly, if subjects
taking allopathic medicine, desire to try traditional therapies as
complementary therapies, they should be allowed to do so under
medical supervision.
It is easy to propose such novel, integrated approached to the
healthcare. But it is not easy, to implement such a project without
passion, dedication, and commitment of various stakeholders.
Moreover, we need to build a different culture altogether, in
which healthy people are counseled for lifestyle changes, and
healthy living habits. In order to prevent the development of
these chronic diseases, the screening for altered metabolism and
counseling for the management of such alterations, should start
early in life. Considering the large number of low birth babies
born in these countries, newlyweds, should be counselled early
on, about the need for supplemental micronutrients during
pregnancy, to prevent fetal origin of adult diseases. Obesity to
a large extent is the driving force, for increased incidence of
diabetes. Therefore, all-out effort should be made, to treat obesity
and obesity-related complications. Similarly, one can recognize
symptoms of altered metabolism, leading to prediabetic state,
and appropriate interventions should be developed to counsel
these individuals, so that diabetes and its complications could be
prevented or postponed.
In developing countries, where no one goes to a doctor unless
one is sick, it is hard to get them, to any of these preventive
programs. Just like there was a global effort, in the prevention
of use of tobacco and tobacco products, a massive educational
program should be developed to educate, create awareness,
of the serious health issues related cardiometabolic diseases.
Every member country of the United Nations has signed a
declaration, to stop increase in the incidence of diabetes by
2030. These high-level committees also have made declaration
to stop the increase in the increase of diabetes in 2025 to 2020
level. These are commendable goals [32-37]. Having said that, I
want to mention, that the various expert committees working on
such task forces, have reported that achieving such sustainable
Million Development Goals (MDGs) are highly unlikely. Making
declarations, developing guidelines, are celebrating World
Diabetes Day, will not solve the problem of these epidemics.
They can be solved only by commitment, and dedicated work by
all the stakeholders. Furthermore, to be effective, such projects
need trained human resources, healthcare infrastructure, and
firm financial commitment. In a short overview like this, we will
not be able to provide all the solutions and answers. We just
have provided a view point, that can be considered by the policy
makers and various governments. We would be glad to be a part
of any such effort.
Recently, the Ministry of AYUSH decided to celebrate National
Ayurveda Day on Dhanvantri Jayanti every year. According to a
report on their website, the “Mission Madhumeha (Diabetes)” was launched on the occasion of first National Ayurveda Day,
celebrated on 28th October 2016 [38]. In announcing this
mission, following statement was issued by AYUSH: This protocol
for “Prevention and Control of Diabetes through Ayurveda” has
been prepared for implementing the “Mission Madhumeha”. An
attempt has been made to bring out the Ayurvedic philosophy
in implementable format. The tables about do’s and don’ts have
been depicted with relevant figures for easy understanding
of the community. The ‘Madhumeha Assessment Tool’ (MAT)
based on Ayurvedic Philosophy has been developed for the first
time for the self-assessment of people with regard to possibility
of diabetes. The intention of developing the Madhumeha
assessment tool is to sensitise people about diabetes, it’s
common symptoms, the Ayurvedic approach of Medodushti
and its symptoms and to encourage them to visit an Ayurveda
hospital, in case of having the score above the threshold. The
specific diet and exercises explained in the protocol would be
useful for the end user to promote self-health. The treatment/
medicines explained for implementation at PHCs/CHCs/ would
provide, the base line for the insurance coverage purpose also.
The charts have been developed in easy downloadable format,
which could be used for developing, posters for display at places
like Educational Institutes, Panchayat and such other relevant
public places. Announcement of this protocol, and the plan to
initiate NCD prevention through AYUSH efforts, are indication
of the Government of India to strengthen primary care at PHCs/
CHCs. We are just expressing our view point on this topic of
great public health importance and suggesting that they should
not only develop Ayurveda approach to this problem, but also
seriously consider the development, of “Integrative Medicine
Approach”, as suggested in this overview.
Conclusion
Cardiometabolic diseases have reached epidemic proportions
worldwide. In the last three decades, obesity has increased by
two-fold and diabetes by four-fold. In the same period in China,
diabetes has increased by 17-fold. It is hard to believe, that an
advanced country like the USA, has the highest prevalence of
diabetes. What is surprising is, the huge difference between
the prevalence of diabetes in adults, versus prevalence of
prediabetes. In China for instance, the estimate of the prevalence
among adults is 11.6% and the prevalence of prediabetes is
50.1%. Twin epidemics of obesity and diabetes is a rapidly
growing public health menace, and if not checked soon, will
result in economic disasters in several developing economies.
In view of this fact, we are proposing an integrated approach to
healthcare, which envisages the use of existing infrastructure,
and trained human resources, and develop a seamless bridge
between the traditional medicine and conventional medicine.
India and China, which have such healthcare platforms, with
some effort, could develop an integrated system of healthcare
delivery, which will revolutionize the way healthcare is delivered
worldwide.
As we mentioned in the article, there are some fractured
attempts, to develop such healthcare in developing countries.
However, it needs more than declaration of efforts, or publishing
protocols. It needs the will, dedication, passion, and commitment
of all the stakeholders. We need to create a whole new culture,
change attitudes of people, provide incentives, use multimedia
platforms, digital infrastructures and smart Apps, to put together
a seamless project, which provides opportunity for individuals
to obtain the benefits of personal, customized health care. Such a
system should integrate diagnostic tools, platforms and emerging
technologies, for early detection of the risks, cluster of risks, and
follow the effect of various therapeutic approaches. Without
such integration, we will not be able to accomplish our goals
of preventing reducing, reversing, or prevention of metabolic
diseases. Guidelines, guidance statements, and protocols, should
be developed by both AYUSH experts, as well as Medical Council
of India, so that practitioners of both the systems of medicine,
agree to use such a protocol. If we take this approach to health
care, we can also develop collaboration with the Global Health
Platforms, as well as the National Institutes of Health, USA. We
have barely touched novel emerging approaches, to healthcare
delivery. If developed properly, with evidence-based knowledge,
these novel integrated approaches, could become the leading
way of healthcare delivery worldwide.
Acknowledgements
Author expresses thanks to Dr. Poornima Murthy, Dr. Krishna
Murthy, The Directors, Prajna Kuteera Ayurvedic Center, Mysore,
India, and Dr. B. R. Pai, Founder Director, Vijay Foundation,
Mysore, India, Co-Founders of the Global Alliance of Traditional
Health Systems (GATHS), and the Mind Body Spirit Society of
India, Mysore, for continued support and collaboration of my
efforts, in developing Integrated Medicine Platforms in India.




Comments
Post a Comment