Juniper Publishers- Journal of complementary medicine

Purpose:Student and clinician burnout in the
health professions have been reported across the education spectrum.
Burnout has been linked to medical errors and decreases in performance.
Increasingly over the past two decades, health professional schools are
implementing mindfulness-based stress reduction courses. Since 2010, the
University of Washington has offered an inter-professional mind-body
skills course to graduate students in the health professions. This study
examines the longer-term impacts of experiential mind-body skills
training on graduate health professional students. The objectives of
this 7-year follow-up study, the first of its kind, were:
1. To determine the value that medical, nursing and
pharmacy students retrospectively attribute to an eight-week mind-body
medicine course, for personal and professional development and for
ameliorating chronic stress
2. To determine the extent to which former students would recommend a similar instructional experience for their peers.
Method:An online follow-up survey was
disseminated in late 2016 to early 2017 to 319 potential respondents who
had taken the course between 2010 and 2017. We filtered the results
into subsets based on the type of student.
Results:Results suggest that most students
retrospectively ascribed beneficial effects to having been exposed to a
variety of meditation techniques, particularly mindfulness and
meditation practices.
Conclusion:Most former students ascribed
beneficial effects to learning mind-body skills during graduate school.
We conclude that such offerings may contribute to the development of
more resilient health professionals. We suggest offering similar
elective mind-body skills courses to students in the health professions
programs (246 words).
Keywords: Mind body skills; Stress mitigation; Resilience; Chronic stress
Student and clinician burnout have been reported
across the medical education spectrum [1,2]. Disconcertingly high rates
of student burnout, defined as constellations of symptoms associated
with a professional practice that can result in emotional and personal
exhaustion and/or disillusionment, have
been reported [3-5]. Within medical, nursing and pharmacy school
environments a myriad of stressors exist that can result in acute and
chronic stress that in turn can lead to personal burnout [6-13].
Clinician burnout has been associated with increases in clinician
medical errors [14-15]and overall decreases in performance [16]. Authors
from the fields of medicine, dentistry,nursing, and social work have
called for multiple approaches to
address the problem of burnout [12,18]. Although burnout was
documented among practicing pharmacists many years ago
[2] little appears to have been done to alleviate the stresses of
pharmacy education or practice.
With increasing frequencies over the past two decades
medical and professional schools have started offering
mindfulness-based stress management and stress reduction
offerings [19-23]. Studies examining the efficacy of mindfulnessbased
stress reduction programs suggest that they can lower
levels of psychological distress in medical students [19,24,25].
An elective mind-body skills (MBM) course was first offered at
the University of Washington (U_) in the 2004-05 academic year.
This was an attempt to ameliorate at least some of the stressors
that are known to interfere with learning in professional school
environments. The course was designed to help students from
the health sciences manage anxiety and stress. Initially, students
were second-year medical students and graduate nursing
students. Later the course was opened to pharmacy students
and, on a space-available basis, to a few students from other
professional schools such as public health and education. The
objective of this study was to determine the extent to which
former medical, pharmacy and nursing students retrospectively
viewed the course’s MBM content and experiences as having been
valuable for their personal and professional development, and
for coping with chronic stress. It was also designed to determine
whether the former MBM students would recommend similar
instructional experiences for others within their profession. The
U_ course, Introduction to Mind Body Medicine – An Experiential
Elective, was adapted from a mind body skills program offered by
the Center for Mind-Body Medicine and was similar to a course at
Georgetown University Medical School [22]. Initially, the U_ MBM
course was offered exclusively to medical and graduate nursing
students. Later, we included pharmacy students. As a ‘conjoint’
course, the founding faculty members were from more than one
professional school. As the course evolved, volunteer faculty also
came from a variety of healthcare professional practices.
The UW mind-body medicine (MBM) course focused on
activities that included various ‘mindfulness practices (mindful
meditation, mindful eating, walking meditation), various other
meditation practices (quiet meditations, shaking meditations,
guided imagery, yoga), as well as discussions about nutrition,
mirror neurons, and spirituality. It was apparent from the
outset that certain activities ‘resonated’ with some students,
but not with others, and vice-versa. Since 2010, depending on
faculty availability, from 2 to 4 concurrent sections of the U_’s
multidisciplinary MBM course were offered during both the
autumn and winter quarters. Each small group consisted of
between 8 and 12 students. Each section of the course met for
eight weeks for 3-hour sessions, with one or two faculty ‘guides,’
most of who were volunteers. Typically, sessions opened with a
brief meditation, a ‘check-in’ and then an activity that provided an
experience aimed at exploring mind-body connections. Listening respectfully without interruptions was the rule. Students were
reminded that they were there to experiences mind-body
practices and to engage in self-exploration, not to fix others.
Modeling the confidentiality of the healer/patient relationship,
we emphasized that anything that transpired during the sessions
was to be held in complete confidence.
Each week’s session focused on students engaging in, one or
more MBM experiences. Each weekly session began with a brief
mindfulness meditation. This meditation was followed by each
participant “checking-in” with a summary of how the previous
week had gone for them. These brief check-ins provided the
group with individual student’s and guide’s overviews of
their successes or challenges during the previous week at
incorporating mindfulness and other mind-body practices,
including exercise, into their daily routines. The check-in allowed
students and the faculty guides to think about and share with
their course colleagues their experiences and related feelings in a
nonjudgmental, supportive environment. The faculty facilitator/
guides participated fully in the group process and presumably
modeled these behaviors, sharing their challenges in keeping
up with the “mindfulness” homework activities. After the checkin
period, the week’s focal point subject was briefly presented,
sometimes with a brief PowerPoint presentation followed by
group discussion and Q&A. The remainder of the sessions, usually
70 to 75% of the time, was devoted to experiential practice with
a variety of meditation techniques and guided imagery. We also
provided a closing meditation at the end of each session.
As a prelude to preparing genograms, students were
encouraged to contact significant family members (such as
parents, aunts, uncles, and grandparents). The goal was to seek
information about family members’ views of family strengths,
beliefs, values, stressors, diseases and relationships about which
the students might not have been aware. A genogram is a family
tree that highlights one’s family’s strengths, beliefs, and values,
stressors, diseases, as well as the extent to which relationships
were close, distant, cut-off and/or conflicted. A review of
genograms is available online [26]. During the last three
sessions, a portion of in-class time was provided for each student
to prepare and then share his or her family’s three-generation
genogram. Over 95 percent of participants chose to present
their genogram and share any insights they might have gained
regarding the extent to which their family’s methods of coping
with and managing stress. Insights about how their experiences
in their families shaped their ability to cope with chronic stress
were shared with the group.
An earlier pre- and post-course effectiveness study
of the UW
MBM course indicated that the course was needed and effective
and that it had lasting short-term impacts. The intervention and
comparison groups, which differed significantly with respect to
anxiety levels at the beginning of the mind-body course (time 1),
were indistinguishable from each other 10 weeks later at the end
of the course (time 2). Three months after the course concluded (time
3), the observed lowered anxiety levels in the intervention
group were sustained [19].
Medical, nursing, and pharmacy students had priority for
registering for the course. Students from other professional
schools were allowed to register on a space-available basis. We
excluded students from other schools from the analyses. After
identifying the pool of health professional students who had
completed the course during the 7-year timeframe between
2010 and 2017, we embarked on the process of locating valid
emails. We finalized a list of 319 “likely valid” emails.
We designed an online follow-up survey to help ascertain
former MBM students’ insights into the effectiveness of the
course for mitigating the effects of chronic stress. The survey
assured potential respondents of confidentiality and was
approved by the U_ Human Subjects Committee. Four related
items queried about attribution of course impacts. These were
1. Would you attribute significant positive long-term
impact(s) on you personally as a result of your having elected
to take our MBM Course?
2. Would you attribute significant positive long-term
impact(s) on the way you professionally practice as a result
of your having elected to take our MBM Course?
3. Would you recommend a similar experiential course of
instruction for friends and family?
4. Would you recommend a similar experiential course
of instruction for your professional colleagues? The four
mutually exclusive, categorical response options were:
a) Absolutely yes
b) Yes, but I expected more
c) Had a slight impact
d) Absolutely not.
The survey also included eight items that asked about the
extent to which the course’s eight MBM components/concepts
helped mitigate the effects of stress.
The eight course components/concepts were: Mindfulness,
Meditation practices, Shaking meditation, Guided imagery,
Mirror neurons, Yoga, Spirituality, and Genograms. The four
mutually exclusive, categorical options were
a) Yes, very effective
b) Yes, moderately
c) Only slightly
d) No, didn’t resonate with me
For each of the eight course components/concepts, the survey
also asked about “the extent to which you have incorporated
course components/concepts into your personal practices.” The
four mutually exclusive, categorical response options were
a) Yes, very effective
b) Yes, moderately
c) Only slightly
d) No, didn’t resonate with me
Finally, we provided a response box for respondents “to offer
an entirely optional reflection about the course.
The survey was disseminated in late 2016 and early 2017
via the UW’s Online Catalyst System to 319 medical, nursing and
pharmacy students who had taken the course during the period
between 2010-2017 and for whom we were able to identify likely
still current contact information. Three automated reminders
were sent to non-responders.
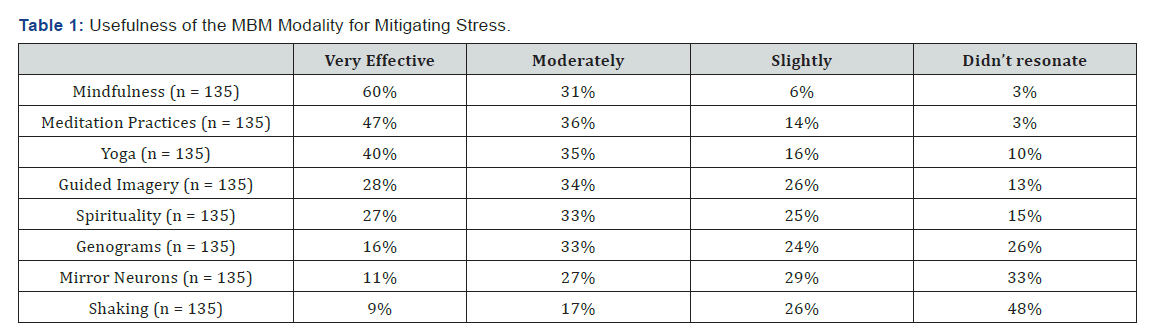
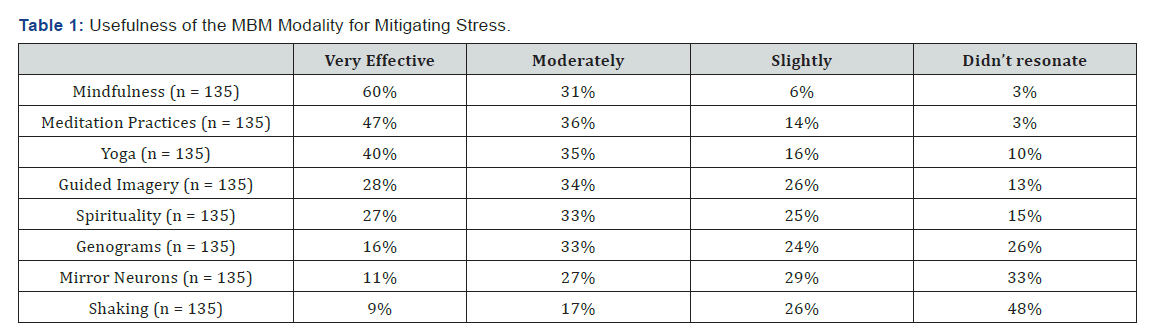
The course provided eight categories of mind/body
experiential activities. These are shown in Table 1 in decreasing
order based on the percent indicating that the category was
“very” effective for mitigating stress. Overall, the most effective
activities for mitigating stress were mindfulness, meditation
practices, and yoga. These were viewed as at least “moderately”
effective by at least 75% of respondents. Guided imagery and
spirituality were viewed as somewhat less effective but were
cited as at least “moderately” effective for mitigating stress by a
majority of respondents. Genograms, information about mirror
neurons, and shaking meditation resonated only slightly or not
at all for the majority of respondents.
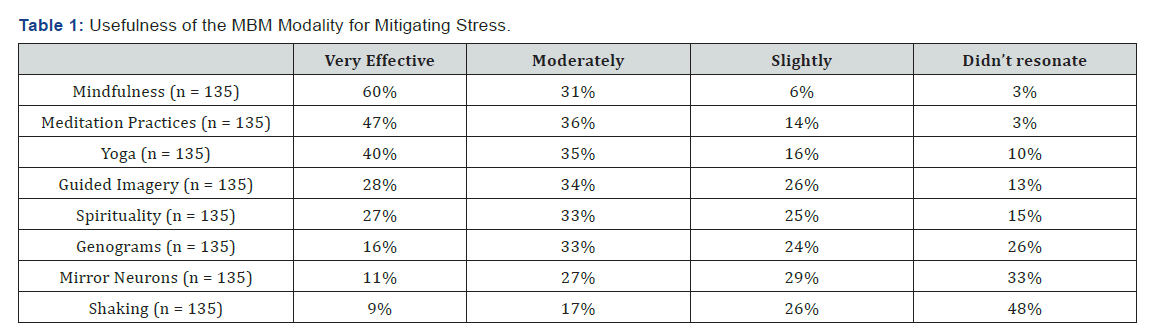
As shown in Table 1, over 75% of responding medical,
nursing and pharmacy students indicated that meditation and
mindfulness practices were “very” or “moderately” effective
for mitigating stress. Yoga, guided imagery, and spirituality
for stress mitigation were viewed as “very” or “moderately”
effective by just over 60% of responding medical, nursing and
pharmacy students. Discussions of the importance of family
history, experiences and values in understanding stress origins,
as reflected in student-generated and shared genograms, was
viewed as “very” or “moderately” effective by 40% of responding
medical, nursing and pharmacy students. The role of “mirror
neurons” in listening to, for understanding the feelings of others
(empathy), and for communicating feelings was cited as “very”
or “moderately” effective by approximately 25% of responding
medical and pharmacy students but by over 60% of the nursing
students. We introduced the concept of mirror neurons by
viewing a NOVA Science Now program that originally aired on
25 Jan 2005. Discussion of mirror neuron implications to mindbody
considerations followed. The NOVA Mirror Neuron Video is
no longer available for streaming from PBS but it is available on
YouTube.
Shaking meditation, promoted by OSHO as kundalini
meditation, involves a series of body movements including
shaking, dancing, and quiet meditation guided by music. It
is a technique that may challenge the ‘comfort zone’ of many
individuals and did not resonate with half of the respondents.
The music is available on CD or online. [27] A number of websites
now promote and present discussions and video demonstrations
of shaking meditation [28,29].

Figure 1 presents the extent to which former medical,
nursing, and pharmacy students reported that the top-rated
“mindfulness” practices helped students mitigate the effects of
stress. The majority of all three types of clinicians indicated that
the course had been “very effective” in helping them mitigate the
effects of their stress (pharmacy students 74%, medical students
54%, and nursing students 53%). Ninety-eight percent (98%) of
medical and 100% of pharmacy respondents indicated that the
course was “very” or “moderately” effective for mitigating the
effects of stress. Eighty-four (84%) of nursing students indicated
that “mindfulness” practices were “very” or “moderately”
effective for mitigating the effects of stress. Two medical student
respondents (2%) indicated that mindfulness did not resonate
with them.
Very similar results were obtained for “mediation practices”.
The vast majority of former medical, nursing, and pharmacy
students reported that “meditation practices” helped them
mitigate the effects of stress. The majority of former medical,
pharmacy, and nursing students indicated that the course’s
meditation experiences were “very effective” in helping them mitigate the effects of their stress. All former pharmacy students
indicated that the course’s meditation experiences had been
either “very” or “moderately” effective at helping mitigate the
effects of stress. Similar percentages for medical and nursing
students were 91% and 84%, respectively. Four percent of former
medical students (4%) indicated that the course’s meditation
practices did not resonate with them.
Figures 2 presents the extent to which former medical,
pharmacy and nursing students attributed long-term course
impacts on their professional practice. When asked whether
as a result of having elected to take this course they would
attribute significant positive long-term impacts on the way
they professionally practice, all former medical, pharmacy
and nursing students responded that the course had at least a
“slight impact” on their professional practice. The percentages
of former medical, pharmacy and nursing students indicating
“Absolutely yes” that they would attribute significant positive
long-term impacts on their professional practice, were 46, 59,
and 32%, respectively.

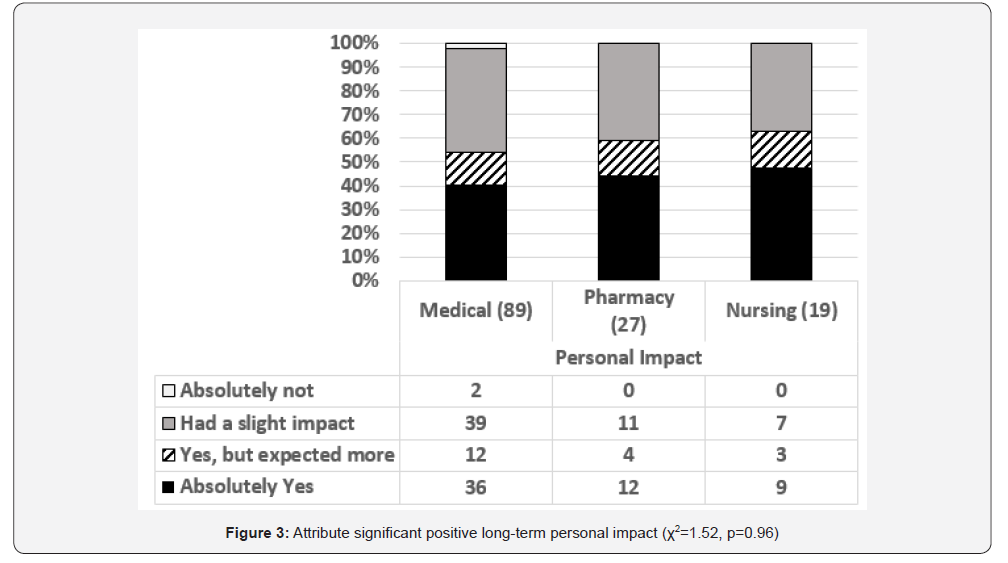
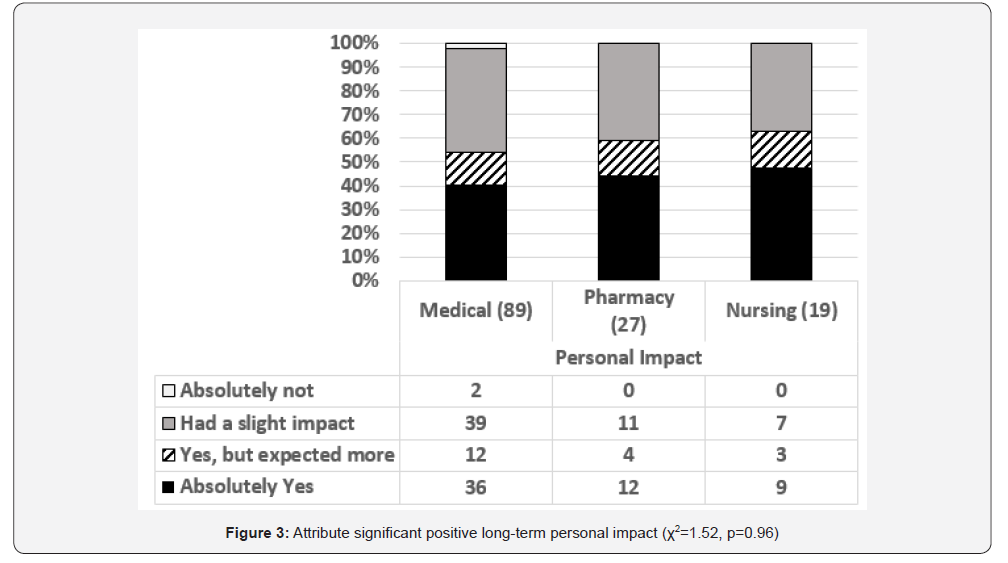
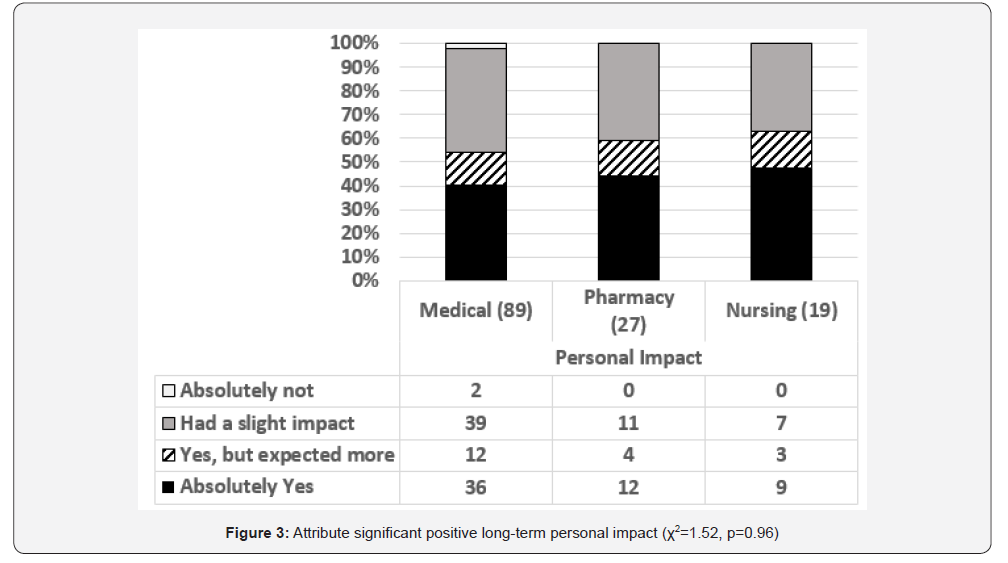
Figure 3 presents the extent to which former medical,
pharmacy and nursing students attributed long-term course
impacts on them. Two medical students (2%) indicated that the
course’s meditation practices did not resonate with them. The
percentages of former medical, pharmacy and nursing students
that indicated “Absolutely yes” that they would attribute
significant positive long-term impacts to the course’s meditation
practices were 40, 44%, and 47%, respectively. The percentages
of former medical, pharmacy and nursing students that indicated
“Absolutely yes” that they would attribute significant positive
long-term impacts or “Yes, but I expected more” were 54, 59,
and 63%, respectively. Respondents from medicine, nursing and
pharmacy highly recommended a similar experiential course
of instruction for their professional colleagues. Over 70% of
the former medical, pharmacy and nursing students responded
“Absolutely Yes” they would recommend a similar experiential course to their colleagues for professional colleagues (medical
72%, pharmacy 85%, and nursing 86%).
Overall, the majority of former health profession students who
participated in the course reported positive long-term impacts.
The most effective of the MBM activities for mitigating stress
were mindfulness, meditation practices, and yoga. Mindfulness
was also the approach that was most commonly incorporated into
personal practices. The majority of respondents also reported
that guided imagery and spirituality were viewed as helpful and
at least “moderately” effective for mitigating stress. Genograms
and information about mirror neurons resonated with less than
half of respondents. By sharp contrast, the shaking meditation
was the least likely to be incorporated into personal practices;
it and was viewed as being “very” or “moderately” effective by
fewer than 30% of respondents. Shaking may have been outside
the comfort zone of some students.
For the majority of former UW medical, nursing, and
pharmacy students, experiences related to the top-rated practice
category of mindfulness indicated that the course had been “very
effective” in helping them mitigate the effects of stress. The vast
majority of respondents viewed mindfulness practices as “very”
or “moderately” effective for mitigating the effects of stress. That
said, two medical students (2%) indicated that the course did not
resonate with them at all concerning the mitigating the effects
of mindfulness. All pharmacy or nursing students indicated
that mindfulness practices were at least “slightly” effective for
mitigating the effects of stress. The overwhelmingly positive
perceptions of the effectiveness of mindfulness practices provide
strong support for offering mindfulness experiences to students
in these health professions, at least as a part of elective offerings.
It should be said that in this study we examined perceptions
of effectiveness, not objective measures of the effectiveness
of mindfulness. A cautionary note; some psychologists,
neuroscientists and meditation experts contend that hype about
mindfulness may be outpacing science [30].
All former pharmacy students and over three-quarters of
former medical and nursing students reported that the course’s
meditation experiences were at least “very” or “moderately”
helpful for reducing the effects of stress. Again, former medical
students were slightly less enthusiastic but still overwhelmingly
positive about the utility of meditation experiences for helping
them mitigate the effects of stress. All respondents attributed
some long-term course impacts on their professional practices.
Likewise, the vast majority of respondents attributed long-term
personal impacts to the course, although 2% of medical students
indicated that they did not attribute any significant personal
impacts to the course. Most importantly, the vast majority of
these former MBM students from the three health professions
indicated “absolutely yes” they would recommend such a course
for their colleagues.
This study provides evidence that mind-body techniques,
particularly mindfulness, when offered in an elective, interprofessional,
small group setting, are viewed positively over time
and may help reduce the high levels of stress encountered within
the healthcare professions. These results suggest that skillsbased
mindfulness courses for health professions students may
serve to reduce burnout in future clinicians. At the University of
Washington we are fortunate to have several health professional schools on the same campus. Some of our nursing students
had many years of clinical experience whereas most medical
and pharmacy students were relatively early in their training.
The result was inter-professional and inter-generational
communication between diverse students from different schools.
From the authors’ point of view, this was an important part of the
small group experience. Insights into the personal viewpoints of
students of other professions, as gained in small group settings,
may help lay the foundation for more mutually empathic ‘team’
approaches to healthcare in the future, but that remains to be
seen. There have been efforts in various institutions to train
students together for technical details of clinical practice, but
evidence-based results regarding health care processes and
patient outcomes have not been definitive [31].
The majority of our former UW students absolutely
recommend that such experiential MBM courses be offered to
help students cope with chronic stress. We hypothesize that
our findings should generalize to other health professions such
as physician’s assistant, dental, physical therapy, rehabilitation
education and the like. Our results support the contention
that experiential mind-body, stress management courses
would contribute to the development of more resilient health
professionals as they enter and pursue their professional
practice years.
Respondents had completed the course anywhere from 7
years ago to 6 months prior. Thus, it is possible that with the
passage of time some of the reported longer-term impacts might
have been slightly lower had all students taken the course 7
years prior to the study. There is likely some attrition bias given
the number of students who were found to have non-working
emails. This may have resulted in an over-representation of
students who took the course more recently.
Health professional education and practice is well known
to be challenging and highly stressful. This study suggests that
providing mind-body medicine experiences during the formative
educational years of health professionals is likely to enhance
their ability to cope with personal and professional stress.
Therefore, we recommend that health professional schools offer
elective, experiential MBM courses. We also recommend formal
training of faculty members to be “champions” of such courses
and provision of dedicated quiet space, stationery supplies,
music, multiple yoga mats, etc.
Multi-institutional follow-up studies that compare and
contrast results from similar courses at different locales, and
perhaps at different points in time, would certainly expand
upon our findings. It would be beneficial to follow-up students
who have completed similar experiential MBM courses over
longer periods of time. These would more precisely quantify how the impressions and effects are impacted by passage of
time and years of clinical practice. Future study designs should
consider incorporating validated burnout, stress, and anxiety
assessments to quantitatively measure the effects of such
courses over longer periods of time and inclusion within the
study designs of comparison/control groups [23]. It would be
useful as well to evaluate with mixed method assessments the
subjective preferences of the students for the different mindbody
practices taught. This would help clarify those practices
from which students would be most likely to benefit. Finally, it
could be useful to know the extent to which those who take such
experiential courses share learned skills with their colleagues,
staff, and/or patients.
The modest resources that elective MBM courses require
to enhance clinician resilience would likely be worth the
investment, at least for those students who feel they are being
overwhelmed by the inevitable challenges and stresses they are
only beginning to encounter; stressors that will persist as they
engage in their chosen professions.








Comments
Post a Comment