Effects of Electro-Acupuncture in Reducing Depression and Anxiety During Heroin withdrawal: A Randomized Controlled Trial- Juniper Publishers
Juniper Publishers- Journal of complementary medicine
Abstract
Opioid misuse and dependency are a public health
crisis. This study examined the effectiveness of an electro-acupuncture
intervention in reducing anxiety and depression among participants with
heroin dependence experiencing withdrawal symptoms during detoxification
stage. The data were from a randomized trial involving 60 adult clients
of an adult drug detoxification program at a detention center in
Shanghai, China. All participants had a diagnosis of heroin dependence.
Participants were randomized to either five times a week,
electro-acupuncture intervention lasting three weeks (totally 15
sessions) or a control group (no intervention). Hamilton Anxiety Rating
Scale and Hamilton Depression Rating Scale were used to assess anxiety
and depression at baseline, at one-week during treatment, at two-week
during treatment, and at post-treatment (three weeks later). Treatment
ended at three weeks later. Post treatment assessment was conducted.
T-tests were used to assess the effectiveness of the intervention. The
electro-acupuncture group improved more on anxiety symptoms than the
control group (P< 0.01). Electro-acupuncture intervention was found
to be effective in reducing anxiety among participants going through
detoxification stage of heroin dependence.
Introduction
Opioid misuse and dependency are a public health
crisis. Opioid prescription rate between 1999 and 2010 has increased by
an estimated 400% [1]. Opioid dependency and the rate of opioid-related
overdoses have tripled since 2000, thus there exists the need for
effective treatment methods [2,3]. Among individuals 12 and older in the
United States, 4.5 million people reported using opioid prescriptions
outside of medical use [4]. This sharp increase in opioid prescription
misuse has led to heroin abuse as ausers transition from prescription
opioids to heroine [5]. Research has shown that those who use
prescription opioids tend to use heroin in the future due to the
accessibility and affordability [6].
Mortality rates involving opioid overdose,
particularly opioid pain relievers and heroin, have tripled since 2000
[2] demonstrateed two distinct but interrelated trends including a
15-year increase in overdose deaths involving prescription opioid pain
relievers and a recent surge in illicit opioid overdose deaths, driven
largely by heroin. Risks associated with opioid and heroin use included a
62% increase in motor vehicle collision risk, toxicity from the drugs
themselves, infections from non-sterile needle use, HIV, hepatitis C,
greater exposure to violence and traumatic injuries [7,4]. Compared to
their non- user counterparts, chronic heroin users are reported to have a
death rate 13 times higher, and chronic opioid users have a rate nearly
15 times higher [8,9]. Additionally, heroin users are 14 times more
likely to die of suicide [8]. Interestingly, Cottler and colleagues
found that many of the deaths occurred among those in treatment-seeking
or treatment-attending individuals [4].
One common method of treatment for opioid use
disorder is substitution medications such as methadone, suboxone, or
naltrexone [10]. Numerous studies have been conducted to study the
efficacy of drug substitution treatment, with most indicating positive
results with long-term treatment. These studies support the idea that
drug substitutes effectively mitigate withdrawal symptoms, promote
treatment retention, and promote positive social activities [11]. Drug
substitution treatment has been so well supported that the Obama
administration proposed a $1.1 billion proposal to further support use
of suboxone to treat people with opioid addictions [10]. However, it
must be taken into account that drug substitutes can lead to negative
outcomes, such as methadone dependence and unintentional overdose [12].
Concomitant use of non-opioid drugs of those seeking treatment is
another problem. Although opioid substitutes effectively block the
effects of opioids that individuals seek, they do not block the effects
of other drugs, such as cocaine, alcohol,
and benzodiazepines [13].
Research is essential in understanding and evaluating
treatment programs specific to opioid dependence and
comorbidities [14]. More research may be conducted to determine
the most appropriate and effective treatment programs to
decrease opioid-related deaths and achieve satisfactory outcomes
to improve daily functioning for individuals who have an opioid
dependence [15]. Multiple factors contribute to relapse of those
seeking treatment, including addiction syndrome, psychosocial
factors, and treatment motivation [16]. Among them, Protracted
Withdrawal Syndrome (PWS) is frequently found among
opioids-dependent patients going through early detoxification.
Protracted withdrawal, is defined as the presence of substancespecific
signs and symptoms as well as the experience of nonsubstance-
specific signs symptoms that persist, evolve, or
appear well past beyond the generally expected initial timeframe
for acute withdrawal. The most common symptoms are anxiety,
depression, and sleep disturbances that can last for weeks or
months. Other possible symptoms include fatigue, dysphoria
(i.e., feeling down or emotionally blunted), irritability, decreased
ability to focus on a task and deficits in executive control
functions that may persist for months. The PWS significantly
contribute to the relapses among opioids-dependent users while
seeking treatment [17]. Therefore, interventions to cope with
withdrawal symptoms are critical to relapse prevention and
treatment success.
The effectiveness of acupuncture interventions for a variety
of health problems have been established for a very long time
[18]. Acupuncture is reported to increase serotonin production
in the central nervous system, and thus reduce depression,
anxiety and subjective distress among patients [19]. It also has
been widely used in pain management [20,21], the treatment of
insomnia [22] stress urinary incontinence [23], the treatment of
insomnia in major depressive disorders [24], and stroke [25,26].
Electro-acupuncture is a type of acupuncture that combines
both electric stimulation and acupuncture. It has been reported
to reduce persistent withdrawal symptoms and prevent relapses
since 1970s [25,27-29]. showed [29] that electro-acupuncture
helps to improve psychiatric symptoms and anxiety and
depression in methamphetamine addicted individuals during
early detoxification and promote rehabilitation of patients.
Clinical experiments and case studies have confirmed its
effectiveness in treating withdrawal symptoms among heroin
users [30,31]. Patients report relief from anxiety, agitation
and depression, especially during the initial detoxification
phase [32,33], as well as decrease in insomnia [34,35]. Studied
[36] the changes of cognitive attention-related brain function
in chronic heroin users during abstinence before and after
electro-acupuncture intervention. Results showed that heroin
users showed attention bias to heroin-related cues, which was
significantly reduced by electro-acupuncture intervention, illustrating that electro-acupuncture could effectively inhibit
the attention bias to heroin and thus can lowering the relapse
rate. Electro-acupuncture thus reduces the physiological and
psychological symptoms in heroin users and helps to manage
withdrawal symptoms [37]. This study used a randomized
controlled design to evaluate the effects of electro-acupuncture
in reducing withdrawal symptoms including anxiety, subjective
distress among 60 heroin-dependent clients in detoxification
stage at a public treatment center for heroin addiction in
Shanghai, China.
Methods
The randomized trial was conducted at an inpatient
rehabilitation unit within a public treatment center for heroin
addiction located in Shanghai, China. All study procedures were
approved by the Yueyang Hospital of Integrated Traditional
Chinese and Western Medicine (affiliated with the Shanghai
University of Traditional Chinese Medicine) Institutional
Review Board.
Participants
Inclusion criteria for study participants were
1. Meeting the diagnostic criteria of opiate dependence
(ICD-10) during the classification of mental and behavior
disorders which formulated by World Health Organization
2. Having heroin dependence for more than half a year,
and the average daily usage was more than 0.5g
3. The age was between 18 ~ 60 years old
4. Having received detox treatment for at least one week
with withdrawal syndrome (including insomnia, depression,
anxiety, body ache, coldness, joint pains, reduced appetite,
constipation, increased heart rates)
5. Negative Morphine urine test
6. Not taking any psychotropic medication including
methadone.
Exclusion Criteria
1. Serious heart disease, serious diseases of
gastrointestinal tract (i.e., gastrorrhagia, stomach cancer,
intestinal cancer, liver cancer), kidney failure, leukemia, and
emphysema
2. Having infectious disease, such as Hepatitis, AIDS, HIV
3. Pregnant and lactating women. These exclusion criteria
are in accordance with the exclusion criteria used in [15]
study.
A total of 60 participants provided written informed consent,
completed baseline assessments, and were randomized to the
Intervention program (n=30) or the Control program (n=30).
Measures
Research physicians assessed participant’s severity of
anxiety using the Hamilton Anxiety Rating Scale [38]. The 14-
item HARS questionnaire has two subscales - psychogenic
and somatic anxiety. It measures somatic (muscular), somatic
(sensory), cardiovascular, respiratory, gastrointestinal,
genitourinary symptoms. The Somatic anxiety subscale measures
muscular, sensory, cardiovascular, respiratory, gastrointestinal,
genitourinary symptoms, and Psychogenic anxiety subscale
assessing anxious mood, fears, depressed mood and insomnia.
Every HARS’s item is rated on a 5-point Likert scale, ranging
from 0 (not present) to 4 (severe). Participants were assessed
at baseline, at one-week during treatment, at two-week during
treatment and at post-treatment (3 weeks later). In addition,
research physicians provided ratings of depression using the
Hamilton Depression Rating Scale [38]. The 21-item HDRS
questionnaire is rated on a 5-point likert scale, ranging from 0
(not present) to 4 (severe).
Treatment programs
Electro-acupuncture intervention (n=30)
The physicians specializing in Acupuncture followed a
standard treatment protocol. The acupuncture needles were
placed on 12 acupuncture points in bilateral arms and legs,
with six acupuncture points on one side of the body [Nei-guan
P6, Shenmen H7, Foot Three Li (near the knee), San-yin-jiao
SP6 (near the foot ankle) bilateral Huatuo Jaji points and Renal
Shu]. The constant current square-wave electric-stimulation
was produced by an EA apparatus (Model G6805-2). The
frequency of stimulation used was 3~5 Hz, rare wave. The
highest intensity of the stimulation was 5 Hz. Each session lasted
for 20 minutes, consistent with Zeng and colleagues [15]. The
intervention was provided once a day, five times a week for 3
weeks. The participants also received regular services provided
at the inpatient unit, including regular breaks in the afternoon
for about one hour, arts and crafts group. Psychological services
such as individual counseling, Narcotic Anonymous (NA) groups,
and group counseling were not provided [39-44].
Treatment as usual group (n=30)
The treatment as usual group received regular services
provided at the inpatient unit. The services included regular
breaks in the afternoon for about an hour, arts and crafts group.
Psychological services such as individual counseling, NA groups,
and group counseling were not provided.
Procedures
Recruitment
Patients were given information about the study and were
referred to the study team if they met preliminary eligibility
criteria for the study. Potentially eligible patients were contacted
by the research team, who described the study and obtained
informed consent. The baseline assessment was conducted to confirm eligibility, with persons meeting all criteria randomized
to either the Electro-Acupuncture group or the treatment as
usual group.
Randomization
Participants were randomized to the treatment group or
control group via random numbers. Sixty participants were
randomized into two groups, with 30 participants in the electroacupuncture
group; and 30 in the treatment as usual group.
Assessment Timeline
Clinical assessments were conducted at baseline, at oneweek
during treatment, at two-week during treatment, and at
post-treatment (3 weeks later).
Results
The characteristics of the two study groups are summarized
in Table 1. The average age was 34.28 years old. The average
educational level was 9.20; 41.7% participants were married,
20.0 % were single, and 38.3 % were divorced. Methods of
drug use were snorting (53.3%), intravenous injection (30.0%),
and injection and snorting both (16.7%). The range of time in
abusing Heroin was 6~222 months. The average heroin-using
time was 64.94±52.73 months. The daily usage of heroin use was
0.5g~4.5g per day, with a mean of 1.17g per day. The average
frequency of usage times was 1~8 times per day. Comparisons
of the two groups at baseline indicated no significant difference
(Table 1). Participants in two groups did not differ on age,
gender, length of Heroin use, and average amount of daily use.
Approximately, one third of the sample were female, while two
thirds of the sample were male. Participants were in their 30s
on average. Participants varied in the length of Heroin use, with
an average length of 50-60 months, averaging four years to five years of history of Heroin use. The average amount of use was
approximately 1.17 grams per day.
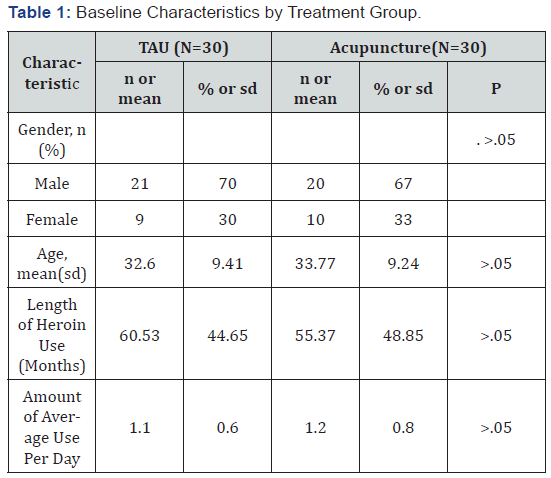
Note: TAU = Treatment as Usual; Continuous variables were analyzed
using one-way ANOVA. Gender was analyzed using chi-square test.
Engagement and Treatment Outcome
Engagement in treatment programs was high, with 30
(100%) participants completing 15 sessions of acupuncture in
the time span of three weeks. The analyses of the other outcomes
indicated significant group effects, with the electro-acupuncture
group improving more than the control group on HDRS, HARS
total anxiety scale, HARS psychogenic anxiety and HARS somatic
anxiety (Table 2). The effect sizes for treatment effect were large
for depression (HDRS, range 1.15 to 2.52), total anxiety (HARS,
range 1.69 to 2.39), large for HDRS subscale of psychogenic
anxiety (2.27 to 2.39) and moderate too large for HARS subscale
of somatic anxiety (0.89 to 1.55).
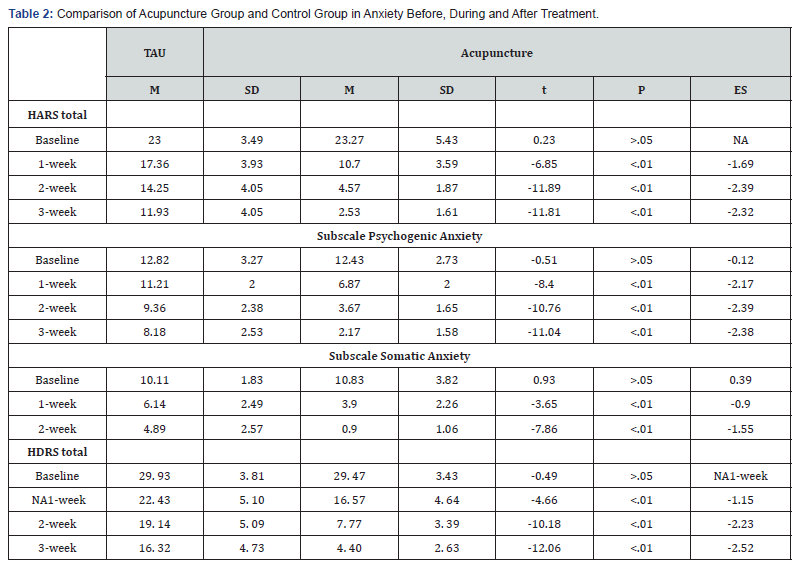
Discussion
This is the first randomized control trial of an electroacupuncture
intervention tailored for individuals with heroin
dependence going through withdrawal symptoms. It examined
the effectiveness of the acupuncture intervention in reducing
anxiety from withdrawal symptoms as compared with the as
usual detox treatment. The effect sizes of treatment were in the
large range for depression, as well as for anxiety. Individuals of
control group had reduced depression as time in detoxification
continued, from 29 points to 16 points on depression rating
scale. Those receiving electro-acupuncture had depression from
29 points to 4 points on depression rating scale. Individuals
of control group also had reduced anxiety, from 23 points to
11 points, while those receiving intervention reduced from 23
points to 2 points. The effect sizes of treatment were mostly in
the large range for anxiety.
The results of this study indicate that those
receiving Electroacupuncture
improved significantly in having less anxiety and
depression than those without acupuncture. Results indicate that
the Acupuncture treatment has a short-term effect in reducing
subjective suffering and as a result, it may increase the chance
of recovery for persons with heroin dependence experiencing
withdrawal symptoms, then they would have been in the
absence of such intervention. This study has several limitations.
The study did not control for expectancy effect (placebo
response) and assessment bias. There was no comparison with
active non-drug treatment condition such as comparison with
psychotherapy condition. Future studies should use a sham
treatment condition to control placebo effect, use a non-drug
active treatment condition as a comparison group, and use
assessors blind to treatment condition. The study only found a
short-term effect of acupuncture and its effectiveness for PWS is
unclear. We caution that this study’s results were obtained from
Chinese ethnic group, and that the results may not generalize to
other ethnic groups, or to individuals with other substance use
disorders, or to those with comorbid mental illnesses. Future
studies on Acupuncture for different ethnic groups, and for
individuals with comorbid heroin dependence and heroin abuse
may be indicated.
Conclusion
In a sample of Chinese adults with heroin dependence, the
electro-acupuncture intervention was found to be effective
than no intervention in reducing depression and anxiety among
participants going through detoxification from Heroin abuse.
The results were fast seen at first week after treatment and
patients continued to improve as treatment progressed until
three weeks later. Results indicate that the intervention may
reduce withdrawal symptoms for this population. More evidence
regarding the acupuncture intervention’s effectiveness for
Opioid abuse is needed to address this question.




Comments
Post a Comment