The Perception of the Patient on the Unit of Intensive Therapy: Literature Review- Juniper Publishers
Juniper Publishers- Journal of Complementary Medicine
Abstract
Introduction: Although the recognition that
the ICU is one of the major responsible for the evolution in health care
in the last century, society continues with a stereotyped view,
considering it as an aggressive, invasive, tense and traumatizing
environment.
Objective:To review the literature to compare the perception of ICU patients about this environment and the professionals who work there.
Methods:A search was made in the scientific
literature through queries in the electronic databases Lilacs, Medline,
Pubmed and Scielo, from the descriptors: perception, patients and
intensive care unit and their correlates in English. We included
original scientific studies of descriptive, experimental or causal -
comparative typology; published between 1995-2015; dependent variable
perception of patients on the ICU; patients who have been hospitalized;
samples composed of individuals older than 18 years and preserved
cognitive ability; clarity in the samples and analyzes.
Results: A total of 63 articles were found, of
which 50 were excluded because they did not meet the inclusion
criteria. Eight articles were used for analysis and discussion, being
grouped in tables
Conclusion: This literature review concludes
that the ICU presents several stressors, both sensory factors and
emotional factors provoked by the experiences and uncertainty of the
outcome in the face of disease. The role of the interdisciplinary team
is a fundamental point to address the resolution of these stressors.
Keywords: Perception;
Patients; Intensive care unit; Articles; Stereotyped view; Comparative
typology; Traumatizing environment; Intensive Care UnitAbbrevations: ICU: Intensive Care Unit; DeCS: Health Sciences Descriptors; MeSH: Medical Subject Headings
Introduction
The Intensive Care Unit (ICU) is a site dedicated to
the care of critically ill patients with clinical instability. Its
approach is interdisciplinary and characterized by frequent use of
diverse technological equipment, aiming at continuous monitoring and
advanced support of life [1-6].
From its conception in the mid-nineteenth century
during the Crimean War, Florence Nightingale realized the need to
isolate the most serious patients and established continuous
surveillance [7-11]. In this context, the ICU acquired the image before
society of a segregating and inhospitable place, directly associated
with death, pain and despair [8].
Although the recognition that the ICU is one of the
major responsible for the evolution in health care and reduction of
hospital mortality rates in the last century, society continues with a
stereotyped view, considering it as an aggressive, invasive,
tense and traumatizing environment. In addition, although the
patient shares the same space with other patients and with health
professionals, the fact of being sometimes decharacterized and
depersonalized, displaced from their familiar, social and professional
environment to an unknown environment, generates in this patient
feelings ambiguous of anxiety, isolation and lack of privacy [4,5,8-14].
Even today, the number of studies that raise the
patient’s impression about this environment, as well as the
psychological and social impacts of ICU admission is limited. The data
present in the literature presents with different methodologies and
visions, and it is necessary to compile this information in order to
have a more linear impression of the patients’ perception about this
care unit. Only then, adjustments and improvements can be made in this
environment and in the professionals working in this unit to better
accommodate patients. In this context, the purpose of this article is to
review the literature to compare the perception of ICU patients about
this environment and the professionals who work there.
Methods
This is a review of the literature, addressing the perception
about ICU by the patients hospitalized in this unit.
Inclusion criteria
Included were: original scientific studies; classified in their
typology as descriptive, experimental or causal -comparative;
published between 1995-2015; considering as an independent
variable the patients’ perception about the ICU; including in
its sample patients who were hospitalized; being composed by
individuals over 18 years of age and with preserved cognitive
capacity. Articles with languages other than English, Portuguese
and Spanish were excluded, as well as a study that expressed the
opinion of third parties about the ICU environment.
Search strategy
Initially the descriptors were established: perception;
patient; intensive care unit. As well as their English-language
correspondents and their synonyms, available in the Health
Sciences Descriptors (DeCS) and Medical Subject Headings
(MeSH). In order to maximize the search were adapted related
words used in pre-retrieved scientific articles.
Respecting the operational differences of each database,
when possible, it was decided to search the “Title” or “Keyword”
primary fields using Boolean operators “or” and “and” and
“connectors” and the term “patient” as the limit. The research
was carried out in the following databases: LILACS, MEDLINE,
SciELO, PudMed. The literature review was carried out from
January to June 2016.
Selection criteria
The articles identified by the search strategy were
independently and blindly evaluated by two researchers LFSS
and BRVNJ, strictly adhering to the inclusion criteria. The
selection of the articles was initiated by the use of the keywords;
followed by the selection of articles by the titles, which privileged
the patient’s perception about the ICU; in the next phase the
pre-selected articles had the summaries read, including studies
that fit the inclusion criteria described above. Finally, due to
the cut-off point established for the selection criteria, a more
experienced researcher analyzed the article in case the two
researchers had a divergence in the decision about including the
study in the systematic review.
Presentation of data
To better understand the data, the articles and their results
were grouped in their own table, containing: author and
year of publication; study design; sample size and outcomes.
Approaching in this table main quantitative as well as qualitative
results on the independent variable in question.
Result
We found 63 articles, of which 50 were excluded because
they did not meet the inclusion criteria. This article includes 13
articles (Figure 1).

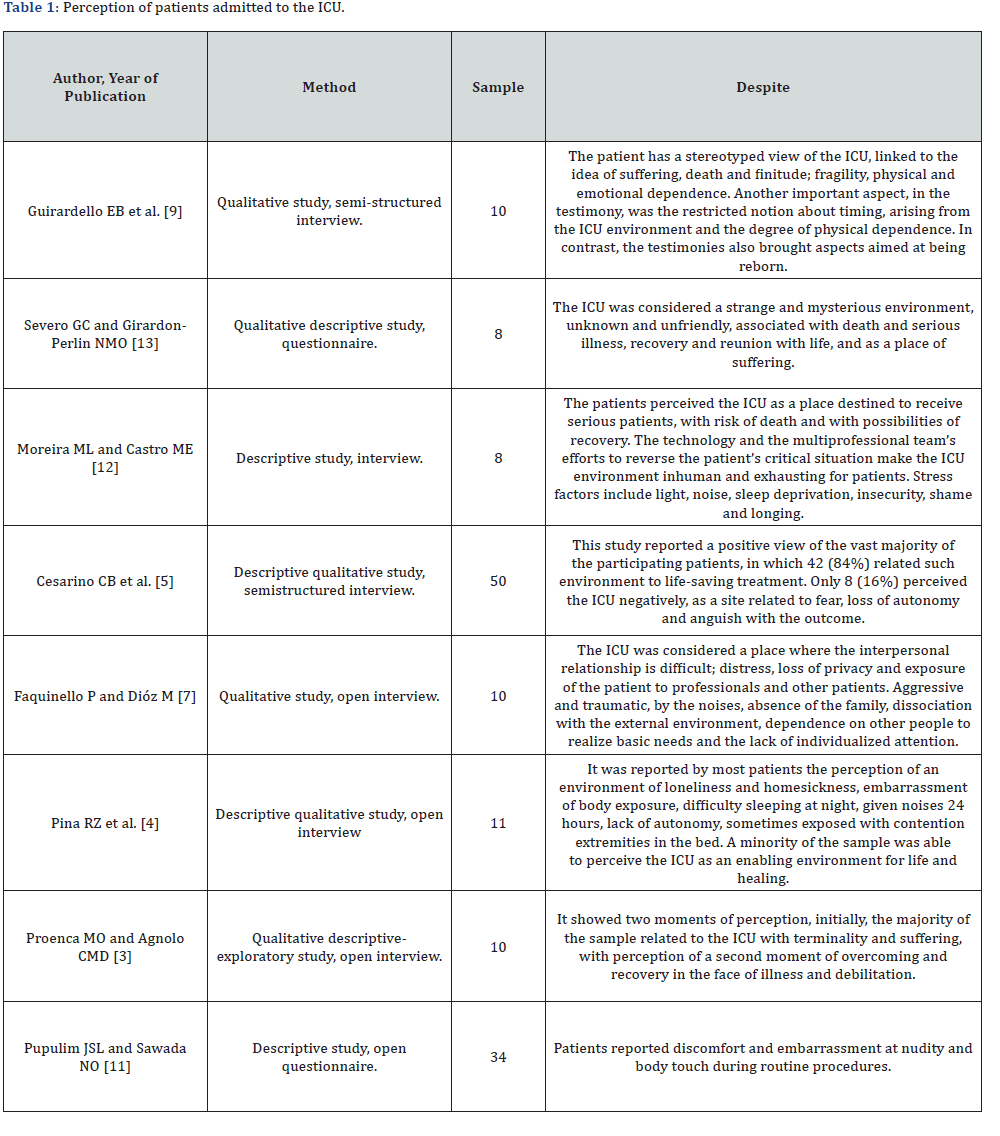
Table 1 expresses the patients’ perception of hospital
admission of the eight articles included in the study. Of these,
6 (75%) of the studies revealed a negative perception generally
aggravated by the structuring of the architectural environment,
however aggravated by the positioning of the professionals
acting there in the face of the suffering and the need of these
patients.
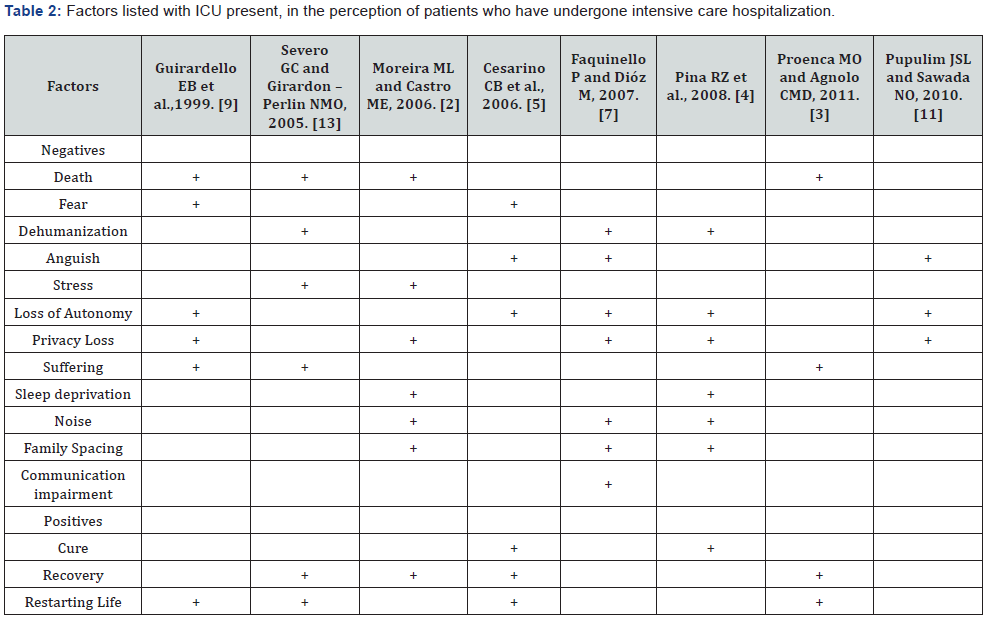
Two studies extolled the therapeutic potential of the
environment, compared to other environmental stressors. The
most perceived negative factors in the ICU were loss of autonomy
and loss of privacy, reported in 5 of the 8 articles included in
this review, followed by death, which was reported in 4 articles
(Table 2).
Discussion
From the present literature review one can perceive the
ambiguity in the patient’s perception about the intensive care
setting. It is noted that a set of intrinsic and extrinsic factors
converge to a positive or negative perception of this environment.
An ICU concentrates the human and material resources
necessary for the adequate care of patients, whose clinical status
requires constant, specialized and uninterrupted health care. It
is considered an environment hostile to human nature because
it enhances physical fragility and emotional vulnerability to the
health-disease process. In confronting the disease and treatment,
patients are faced with circumstances that interfere with their
lifestyle, in addition to living with people who are not part of
their social structure [8,13].
The main objective of an Intensive Care Unit is to restore
in severe patients the functioning of one or more severely
altered organ systems until the underlying disease is adequately
compensated or until the physiological parameters reach
acceptable levels. In order to do so, the technological advance
in this sector aims to integrate the technology to the care,
dominating the scientific principles that base its use and at
the same time supplying the therapeutic needs of the patients
and preserving their individuality [8,15]. In this context, the
urgency and the invasiveness of the procedures performed are
almost always perceived to patients by feelings such as hostility,
coldness and impersonality, making it necessary to reflect on the
real role of the human resource allocated in the ICU, if the must
it be purely technical excellence, or does it require more and
more sensitivity in transferring to the feelings of others, always
respecting the professional callosity that will make the execution
of their office possible?
Among the characteristics of this type of unit, it includes the
intensive care, patients that present risk of death, in addition
to the physical structure composed of several equipment and
human resources. These characteristics associated with the
stereotypes brought by the patients and the coexistence with
other people in serious condition, make the perception of
the own death as a concrete possibility [14]. Several authors
point out that patients perceive the Intensive Care Unit as an
environment related to death [5-8, 10,12,15,16]. In the reports
collected in a hospital in the southwest of São Paulo, Brazil, the
fear of dying is intimately related to the lack of knowledge and
uncertainty of what is happening in this environment and that
previous experience with the suffering of some known in the
Unit contributes to accentuate this feeling [6].
Likewise, in the studies conducted in a coronary unit
in São
José do Rio Preto/SP [8] and the Federal University of Maringá
[7], the fear of dying was a symptom reported by some of the
interviewees [7, 8]. The very term “intensive therapy” already
causes an emotional overload, associating this environment with
the finitude of life [8]. It was also reported by Severo GC and
Girardon-Perlini NMO (2005) that fear of death is considered as
part of the dying process and therefore many of the participants avoided
speaking the word “death”, evidencing the denial of this
process and the difficulty of the patients to deal with the finitude
of life [16].
In ICUs patients usually stay together, in the same physical
space or with partitions that make it possible to see, hear and
perceive everything that happens around them [16] and begin
to develop considerable sensitivity to what is happening around
them, given the stress situation faced in the ICU [10]. In contrast,
stressors, almost existential in the routine of the ICU, such as fear,
death and pain, it is well known that the team’s attitude towards
such concerns is decisive in the way in which these feelings will
be perceived and they will influence or not the structural and
functional recovery of organic and psychic systems.
The use of equipment, probes, drains and catheters makes
the patient feel uncomfortable, but considers them important
for their recovery [16]. On the other hand, routine activities in
the ICU are stress-generating factors and placed as extremely
negative because they result in a noisy, inhospitable and highly
stressful environment [10]. The strange machinery, constant
deprivation, sleep interruptions, sensory overstimulation, thirst,
pain, nasal feeding, ventilator breathing, continuous monitoring
and signs, catheters, invasive procedures, artificial lighting,
conversations, and lack of privacy trigger the patient’s sense of
anguish, making them perceive the environment as unfriendly
[5, 6, 10].
Corroborating the above, this feeling of anguish was cited
by patients in several studies as a negative factor in their stay
in the ICU [5-8,10,12,15,16]. The difficulty of understanding the
intensive physical environment caused by sedation or organic
weakness are factors that intensify this perception and show
the stigma attributed to this sector [10]. In the study conducted
by Moreira e Castro (2006), the interviewees considered that
the technology and the multiprofessional team acting in the
eagerness to reverse the patient’s critical situation make the ICU
environment inhumane and exhausting [15].
Still regarding the feeling of anguish experienced by the
patients, the interviewees in a university hospital in Campinas-
SP explained about the prison feeling for the equipment, loss
of the notion of time, lack of natural light and alteration of the
sleep-wake cycle, and exclusion from discussions about their
treatment [12].
The illness condition also generates feelings such as
incapacity, dependence, insecurity and loss of control over
oneself that make hospitalized patients consider hospitalization
a factor of depersonalization because they recognize the difficulty
in preserving their identity, individuality and privacy [7].
The perception of deprivation of autonomy, of freedom, lack
of mastery of the situation coupled with physical weakness,
and dependence, leads to a state of inactivity and arises for the
patient as part of a reality that is difficult to accept mainly in
the acute phase of the disease [5]. In this context, Faquinello
and Dióz emphasize that the principle of autonomy must be
considered, guiding the actions of professionals working in this
area [10].
Associated with deprivation of independence, the
hospitalized patient feels more needy, fragile, insecure and
lonely. Although they are in the company of the health team and
other inmates, respondents in several studies felt that being
away from family members, their home and their routine, made
them feel alone and unprotected [5,7,16]. In this sense, Severo
and Girardon-Perlini understand that the presence of a relative
is emotional security for the hospitalized patient, besides being
a preventive measure to the problems related to the psychosocial
integrity of the patient [16]. The lack of privacy, especially at
bath time, was another point addressed in the articles studied
[8,14]. Pupulim & Sawada [14], emphasize that in health care
the violation of a person’s privacy can occur in varied forms and
at different levels, such as information, personal and territorial
space, body, psychological and moral field.
An important and unavoidable complaint cited in the study
by Guirardello et al. [12] is pain, caused by several factors, such as
them, procedures and, often, physical discomfort itself. However,
pain is difficult to analyze because it has a subjective, individual
and emotional character, that is, it has a direct relationship with
what each person is, feels and experiences [12,15]
Although many studies show that the common understanding
about the ICU characterizes it as an impersonal and inhumane
environment, destined to patients on the verge of death, besides
connoting to the professionals there acting, coldness and
insensitivity, the articles analyzed showed that, after the period
of hospitalization, the patients began to relate the ICU with
recovery, overcoming and synonymous with life. In addition,
they perceive and recognize the dedication, the continuous care
and in a complete way, the humanization of the care provided by
the health team [6-8,10,12-15].
It is observed that when the patient identifies the team as
a source of safety, protection and care, he begins to establish a
relationship of trust with the professionals and to make sure
that he is being cared for. Thus, even distant from the family,
the patient feels supported and assisted, contributing to a
positive image and satisfactory perception about the period of
hospitalization [7,16].
At present, several studies address the need to adopt a
humanized posture by the interdisciplinary team, such postures
come from structural adjustments in the unit, such as placement
of windows, televisions and clocks near the patient’s bed, until
a hearing of the demands and complaints experienced by the
patient and family, as well as more complex measures such as
immersion of family members 24 hours in the unit or programs
of continuing education in waiting room and patient care in
groups or in external environments the unit or idealized to host
or include this patient [17-20].
The experience of hospitalization and the disease itself put
the human being in a crisis situation. It is fundamental that the
intervention in the ICU preserves both the physiological and the
mental health of the patient, helping in its full recovery through
a humanized care and allowing it to perceive the experience
in the ICU in the best possible way. Further studies are
needed to evaluate the impact of adaptive measures to reduce
negative experiences during hospitalization and to address the
importance of physiotherapy in this context.
Conclusion
The present review concludes that the ICU presents several
stressors, be they sensory factors such as noise, lightness and
invasive procedures that bring pain, as well as emotional factors
provoked by the experiences and uncertainty of the outcome in
the face of disease.
The role of the interdisciplinary team seems to be the
fundamental point to delineate if the patient exposed to these
stressors will understand such experience with an example
of overcoming and new life opportunity or as a traumatic
experience that mostly leaves physical and psychic.
For more Open access journals
please visit our site: Juniper Publishers
For more articles please click
on Journal of Complementary Medicine & Alternative Healthcare




Comments
Post a Comment