Acute Hydrothorax Diagnosed Through Scintigraphy in a Patient on Peritoneal Dialysis- Juniper Publishers
Juniper Publishers-Journal of Complementary Medicine
Abstract
Acute hydrothorax after peritoneal dialysis (PD) is
uncommon. Differential diagnoses of various clinical conditions that can
result in pleural effusions are necessary. Erroneous diagnoses and
subsequent management not only increase the time required for resolving a
problem but also deteriorate a patient’s clinical condition. We report
the case of a 55-year-old woman who received regular PD due to chronic
renal failure. She experienced diffused abdominal pain 2 hours after PD.
Furthermore, dyspnea developed the following morning. A chest plain
film revealed a massive right-sided pleural effusion. Peritoneo-pleural
communication caused by a diaphragmatic defect was diagnosed rapidly
using lung perfusion scintigraphy.
Our patient, a 55-year-old woman, had a history of
hypertension and chronic glomerulo-nephritis-related uremia. She had
undergone peritoneal dialysis (PD) catheter insertion in September 2014
and started receiving continuous ambulatory peritoneal dialysis (CAPD)
twice daily 1 month after catheter insertion. She experienced
intermittent abdominal pain 3 months after the insertion. No fever or
dyspnea were noted with the pain. However, a decrease in ultrafiltration
volume or rate after the PD session was noted by the patient herself. A
review of her medical history did not reveal recent trauma to the chest
or previous diaphragmatic surgery. However, shortness of breath was
noted 1 day later; hence, she presented to the emergency department
(ED). Tachycardia (104bpm) and elevated blood pressure (185/111mmHg)
were noted in triage, and her respiratory rate was 22 breaths/min with
98% oxygen saturation. No chest pain or abnormal findings in the
electrocardiogram were noted during her ED stay. Laboratory results did
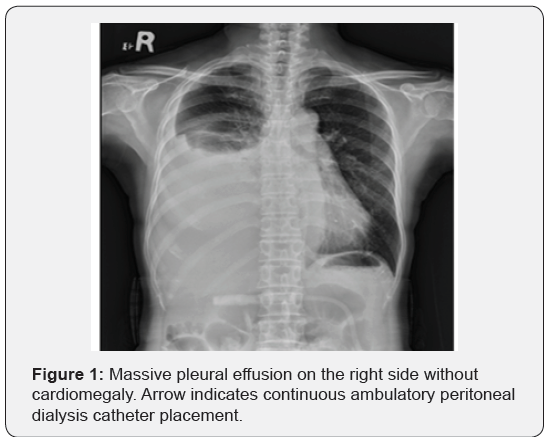
not reveal leukocytosis or acidosis. A chest X-ray revealed a massive
right-sided pleural effusion (Figure 1). Pleurocentesis was suggested,
but the patient refused. We analyzed the dialysate instead of a sample
of the pleural effusion fluid; no evidence of infection was found. We
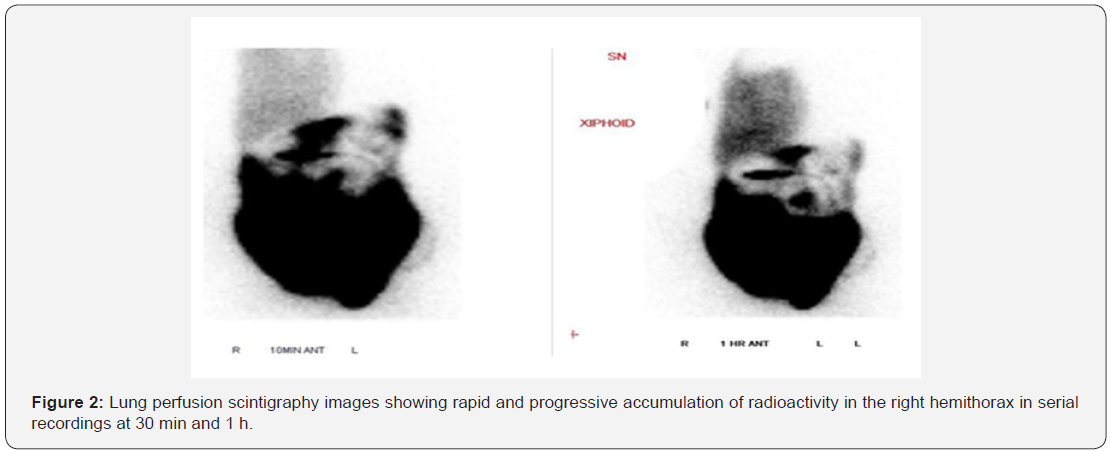
arranged lung perfusion scintigraphy, 5 mCi of Technetium-99m macro
aggregated albumin (Tc-99m MAA) was injected into the PD fluids, and a
rapid accumulation of radioactivity
in the right hemithorax was observed in the images recorded at 30 min
and 1 h after PD (Figure 2). Thus, peritoneo-pleural communication
(right side) caused by diaphragmatic defect was diagnosed. PD was
discontinued immediately and video-assisted thoracic surgery with
thoracoscopic diaphragmatic fundoplication and pleurodesis was provided 2
days later. The patient was discharged uneventfully without the
recurrence of pleural effusions during a 3-month follow-up.
Discussion
Hydrothorax-related to PD was first reported in 1967
by Edward and Unger [1]. The reported incidence rates of
hydrothorax-related PD vary from 1.6% to 10% [2,3]. The
incidence rate in new PD patients is <2% [2]. Pleural effusions
are usually observed on the right side, presumably because
the left side has diaphragmatic protection provided by the
heart. Clinical symptoms of pleural effusions include sudden
dyspnea, decrease in ultrafiltration rate, and pleuritic chest
pain. One study reported that approximately 25% of patients are
asymptomatic [4]. In patients with recurrent unilateral pleural
effusions or acute respiratory distress after dialysate infusion,
trans-diaphragmatic leakage or peritoneal fistulae should be
considered. When transudative pleural effusions are confirmed
using Light’s criteria in patients receiving PD, pleural effusion
glucose levels can aid diagnosis. Some authors use a cutoff
point of 300mg/dL of pleural effusion glucose for diagnosis
[5], whereas others consider a pleural-fluid-to-serum (PF-S)
glucose gradient of >50mg/dL, with a sensitivity of 100%, as an
indicator [6]. A relatively objective measurement revealed that
a PF-S glucose ratio of >1 is consistent with pleuroperitoneal
communication because all other causes of transudative pleural
effusions have similar or lower glucose concentrations in the
pleural fluid compared with the serum (ratios of ≤1) [7]. Any
image survey alone is insufficiently sensitive for detection. In
most cases, peritoneo-pleural fistulae are diagnosed through
scintigraphy or radionuclide scanning (for example, Tc-99m
DTPA), with sensitivities of only 40% to 50% [8,9]. However,
patients receiving CAPD who present with acute shortness
of breath or recurrent unilateral pleural effusions should be
examined through peritoneal scintigraphy to eliminate the
possibility of a pleuro-peritoneal leak. Several therapeutic
approaches can be adopted, including temporary discontinuation
of PD, tetracycline instillation into the pleural space, and surgical
patch grafting of the diaphragmatic defect. The strategy required
to manage the effusion depends on the clinical condition of the
patient; however, in all cases, immediate interruption of the PD
is required. Surgical intervention was provided to this patient
because she showed rapid accumulation of radioactive material
in the right hemithorax.
Conclusion
In patients who receive regular PD, sudden accumulation
of pleural effusion can be diagnosed by minimal invasive
scintigraphy instead of pleural effusion tapping. Rapid diagnosis
can help us decide whether to discontinue PD to prevent
deterioration.




Comments
Post a Comment