An Amazing PFS with Icotinib in a Lung Adenocarcinomas Patient Harboring Rare Complex Gene Mutations: G719C/ S768I- Juniper Publishers
Juniper Publishers- Journal of complementary medicine
Abstract
Background and purpose: Nowadays, epidermal
growth factor receptor tyrosine kinase inhibitor (EGFR-TKI) targeted
therapy has developed to be the standard therapy for patients with
advanced lung adenocarcinomas harboring common EGFR mutations. But the
efficacy for the so-called rare and especially for the very rare complex
EGFR mutations is not clear.
Methods: We describe a case of a 61-year-old
male with advanced lung adenocarcinomas harboring rare complex EGFR
mutations (G719C and S768I), and observe the clinical efficacy of
icotinib, We discuss our case with other literatures.
Results: he has a good clinical response to icotinib. His progression-free survival (PFS) has reached to 36 months.
Conclusion: It may suggest that lung
adenocarcinomas patients harboring rare complex gene mutations (G719C/
S768I) have relatively good efficacy and safety to icotinib.
Keywords: PFS; icotinib; rare; complex gene mutation; G719C; S768I
Abbreviations:
EGFR-TKI: Epidermal Growth Factor Receptor Tyrosine Kinase Inhibitor;
PFS: Progression-Free Survival; NSCLC: Non-Small Cell Lung Cancer; CT:
Computed Tomography; ALT: Alanine Aminotransferase; AST: Aspartate
Aminotransferase; Scr: Serum Creatinine
Introduction
Lung cancer is the leading cause of cancer related
mortality worldwide and non-small cell lung cancer (NSCLC) represents
80% of all lung cancers. EGFR mutations are found approximately in 10%
to 20% of the Caucasian population and from 30% to 60% of the Asian
population with NSCLC [1]. In recent years, EGFR-TKIs have improved to
be the standard therapy for NSCLC with common EGFR mutations. However,
the efficacy for rare complex EGFR mutations is not clear [2]. We herein
report a case of a patient with adenocarcinoma of the lung exhibiting
two rare mutations, G719C in exon 18 and S768I in exon 20. He was
treated with icotinib, and his PFS has reached to an amazing number (36
months).
Case Report
A 61-year-old man with a 40-pack-year smoking history
was admitted to our hospital in August 2015 because of an incidentally
found mass in the lung. He underwent the right nephrectomy because of
his right renal cyst in 2000. Physical examination revealed nothing of
significance in the chest, abdominal regions, nor in the extremities. A
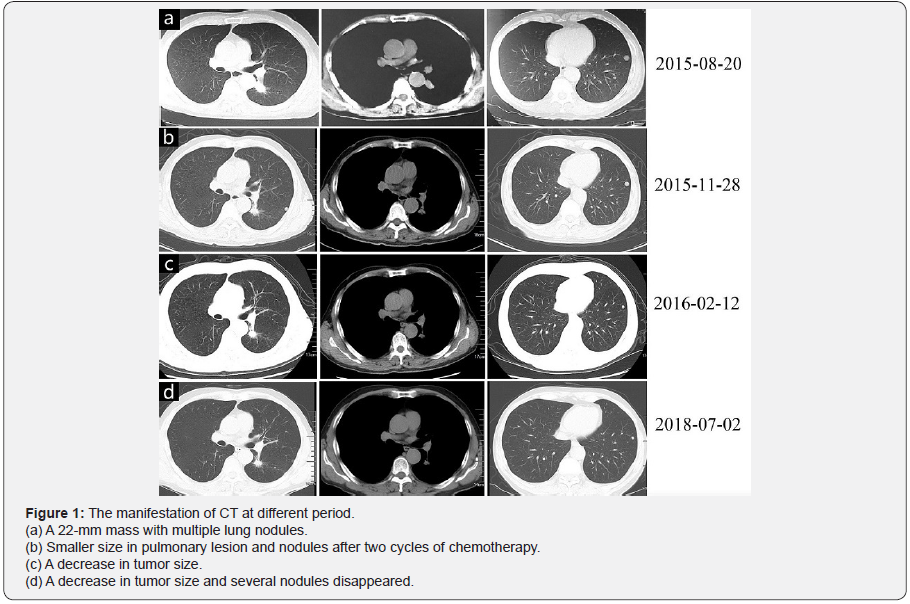
computed tomography (CT) scan of the chest (Figure 1a) on 20, August
2015 revealed a 22-mm mass in the left lower lobe with multiple lung
nodules in both lung fields without
mediastinal lymph nodes enlargement. Fiberoptic bronchoscopy was
performed in our hospital. He was diagnosed advanced lung
adenocarcinomas. He had two cycles of chemotherapy (pemetrexed 500mg/m2,
day 1, oxaliplatin 130mg/m2, day 1). The levels of alanine
aminotransferase (ALT, 174.5U/L) and aspartate aminotransferase (AST,
106.4U/L) in the serum were significantly increased within one month
after the first cycle of chemotherapy. Fortunately, in his specimen of
brush biopsy, rare complex EGFR mutations (G719C in exon 18 with
abundance 11.65% and S768I in exon 20 with abundance 18.46%) were
detected by the approach of next-generation sequencing. Then he received
EGFR-tyrosine kinase inhibitor, gefitinib, as the second line treatment
in a standard dose of 250 mg per day from October 2015. But he
underwent severe diarrhea and serious hepatic damage, his levels of ALT,
AST and serum creatinine (Scr) rose up to the highest peak (ALT 488U/L,
AST 358U/L, Scr 157umol/L) after three weeks. Then his drug usage was
stopped for about half a month and dose of 250 mg per day was reduced to
250mg every other day. Diarrhea and hepatic damage relieved half a
month later. His chest CT (Figure 1b) on 28 November 2015, showed little
smaller size in pulmonary lesion and multiple pulmonary nodules Then
gefitinib was changed to icotinib in a standard dose of 150
mg three times a day from December 2015 and no diarrhea and
other complications occurred from then on. His levels of ALT and
AST went back to normal and a follow-up chest CT (Figure 1c) on
February 12, 2016, showed a decrease in tumor size as well as the
multiple pulmonary nodules. His chest CT (Figure 1d) on July 02,
2018, showed smaller size of the cancer and several nodules disappeared
without diarrhea or hepatic damage. Now the patient is
in good condition with follow-up.
Discussion
Exon 19 deletions and L858R point mutations in exon 21,
are classical mutations, constituting 80-90% of EGFR mutations
[3]. They are confirmed as sensitive mutations to EGFR-TKIs.
With the clinical application of more sensitive and precise tumor
genotyping systems, rare EGFR mutations, such as various point
mutations, insertions, and double mutants, are also frequently
encountered in routine clinical practice. S768I, a mutation in
exon 20, is one of those rare mutations and occurs approximately
1-2% in EGFR mutant of lung cancers [4]. G719C is also a very
rare mutation in exon 18 of EGFR gene and is not often described
in literatures. Compound EGFR mutations, defined as double or
multiple independent mutations of the EGFR tyrosine kinase
domain, comprise 14% of all mutations identified during routine
sequencing of exons 18-21 of EGFR [5]. But the rare compound
mutations with G719C and S768I are absolutely rare.
EGFR-TKIs have effective in the treatment of non-small cell
lung cancer with common EGFR mutations. Nowadays, Gefitinib,
erlotinib, afatinib and icotinib have been used in clinical practice.
But the relationship between rare EGFR mutations and sensitivity
to EGFR-TKI in NSCLC remains controversial. A retrospective
analysis by Baek et al. [6] reported that patients with rare or
complex mutations had inferior response and survival when treated
with EGFR-TKIs compared with patients harboring common EGFR
mutations. Chiu et al [7] indicated that the type of EGFR mutation
was an independent predictor of EGFR-TKI treatment response.
They proved patients with uncommon mutations had significant
shorter PFS (median, 7.7 vs 11.4 months; p < 0.001) and overall
survival (median, 17.2 vs 27.8 months; p<0.001) than that of
patients with common mutations.
By contrast, one prior clinical case of an EGFR S768I mutant
of lung adenocarcinoma reported apparent sensitivity to gefitinib
with a PFS more than 15 months [8]. Hellmann et al. [9] reported a
case which provided conclusive evidence that EGFR S768I mutant
of lung adenocarcinomas was sensitive to erlotinib. Pasello et
al. [10] proved that afatinib seemed to be effective in rare and
complex mutations. Based on these findings, we hypothesized that
cases with different type of mutations had different response to
EGFR-TKIs.
In our case, the patient harboring the rare mutations (G719C/
S768I) received gefitinib as the targed therapy, but severe diarrhea
and hepatic damage occurred. Then he started to take icotinib
and achieved stable disease and his PFS was 36 months. From
our case and literatures, it confirms that, the described complex EGFR mutations (G719C/ S768I) have relatively good sensitivity
to icotinib. It is expected that such rare complex mutations may be
more frequently detected with wider adoption of NGS-based tests.
More dedicated efforts are needed to clarify their biologic effects
on disease course and drug responsiveness.




Comments
Post a Comment